Eosinophilic esophagitis
Once considered rare, eosinophilic esophagitis (EoE) is now a leading cause of dysphagia and food impaction in young adults. EoE is a chronic, immune-mediated condition that affects the esophagus, often triggered by food allergens or environmental exposures. It leads to esophageal inflammation, tissue remodeling, and, over time, can cause strictures that impair swallowing. EoE is now recognized as a growing clinical concern, particularly in Western countries.
How common is EoE?
EoE has seen a marked rise in prevalence, with global estimates now exceeding 140 cases per 100,000 people.
What symptoms are often associated with EoE?
Symptoms vary by age. Infants and toddlers may present with feeding difficulties, poor weight gain, or failure to thrive. In school-aged children, common signs include abdominal pain, vomiting, and dysphagia. Adolescents and adults often report dysphagia, particularly with dry or dense solid foods, and may experience food impaction.
What tests are used to diagnose EoE?
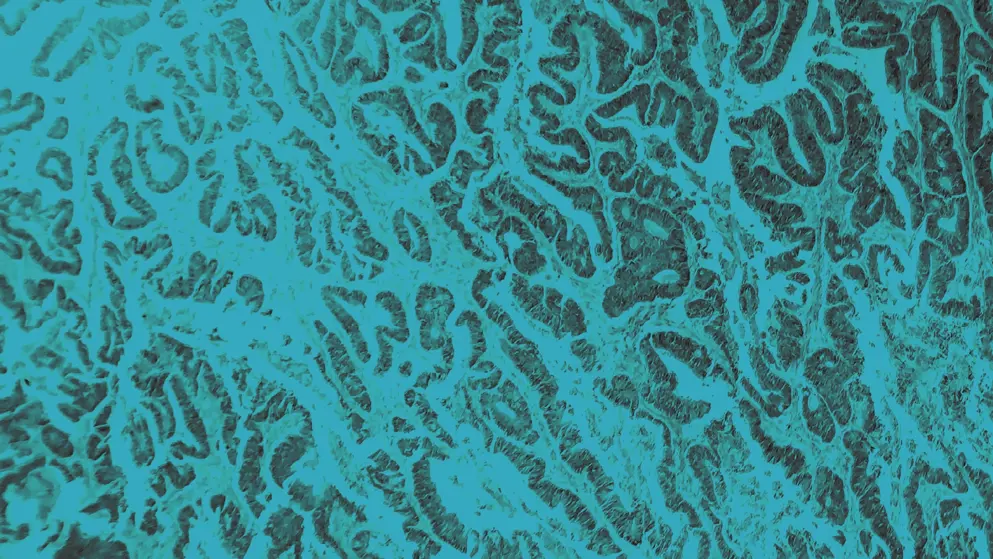
Diagnosis relies on upper endoscopy with biopsy. Endoscopic findings may include rings, exudates, furrows, and strictures, though the mucosa can appear normal. Histological confirmation of eosinophilic infiltration is essential. Additional tests, such as serum immunoglobulin E or eosinophil counts, may support an atopic profile. Non-invasive tools – such as the esophageal sponge – are emerging as alternatives for monitoring inflammation.
What treatment is available for EoE?
Management includes dietary restrictions, proton pump inhibitors, and topical steroids. In more severe cases, biologics targeting type 2 inflammation may be considered. Esophageal dilation can help relieve symptoms in patients with strictures.
Developed by EPG Health for Medthority, independently of any sponsor.

