Heart failure
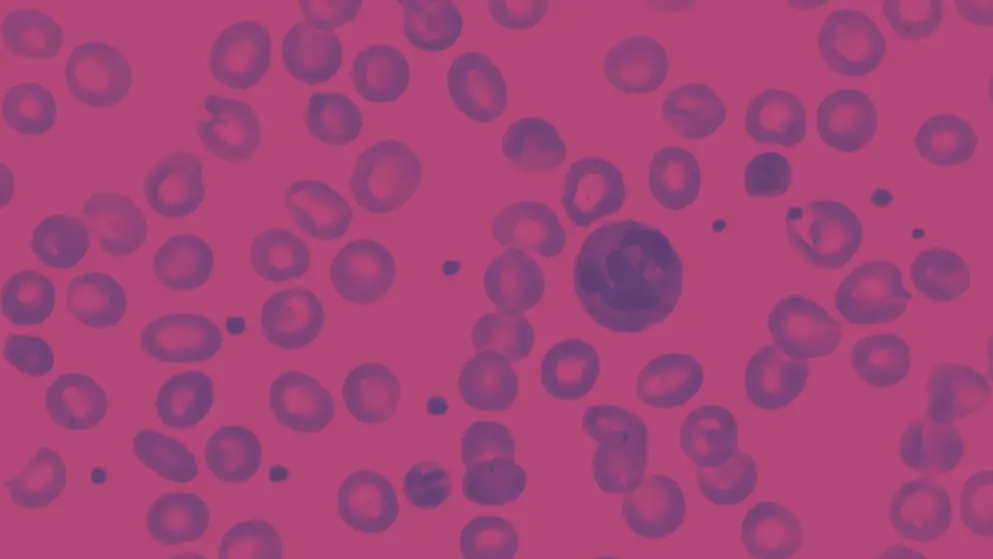
Heart failure (HF) is a cardiac condition caused by structural or functional impairment of ventricular filling or ejection of blood. It is classified based on left ventricular ejection fraction (LVEF) into four categories: HF with reduced EF (LVEF ≤40%), HF with mildly reduced EF (LVEF 41–49% with clinical evidence of HF), HF with preserved EF (LVEF ≥50%), and HF with improved EF (LVEF >40% in patients with previously documented LVEF ≤40%).
How prevalent is HF?
HF is a leading cause of morbidity, affecting over 60 million people worldwide. Its prevalence continues to rise, driven by aging populations and increasing rates of comorbid conditions, such as hypertension, diabetes, and obesity.
What conditions are associated with HF?
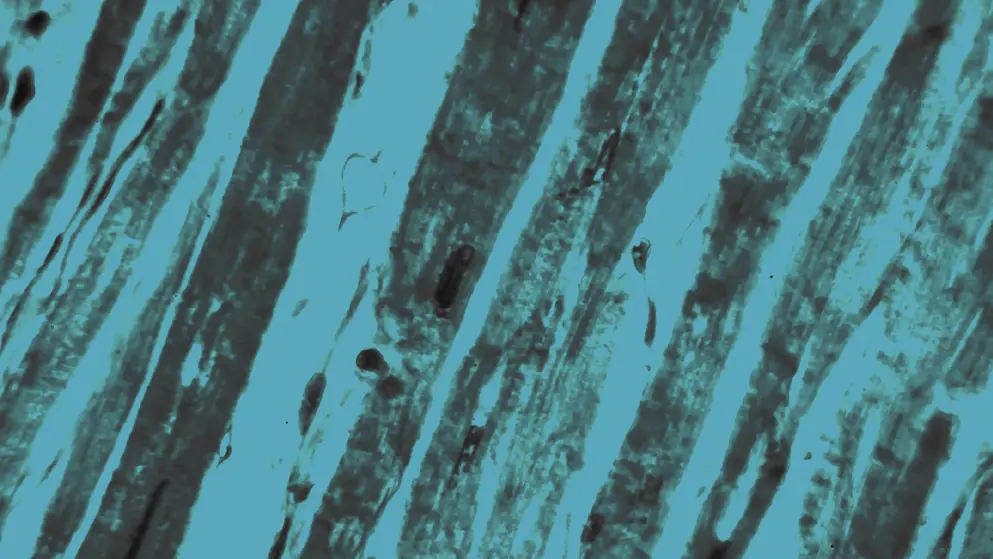
HF is often associated with various underlying conditions that can either directly damage the myocardium or increase cardiac workload. Ischemic heart disease is the most common cause of HF; however, other conditions like myocardial infarction, hypertension, cardiomyopathy, myocarditis, arrhythmias, diabetes, and obesity are also risk factors.
What are the current guidelines for managing HF?
The American College of Cardiology (ACC) and American Heart Association (AHA) guidelines are used for the classification and diagnosis of HF, emphasizing prevention and early intervention. Pharmacological treatment recommendations include renin–angiotensin system inhibitors, beta-blockers, mineralocorticoid receptor antagonists, and sodium-glucose cotransporter-2 (SGL2) inhibitors, as well as diuretics for symptom relief. Non-pharmacological treatment strategies include lifestyle changes and patient education. Device therapy, including implantable cardioverter-defibrillators and cardiac resynchronization therapy, is recommended for specific patients. In advanced cases, options include mechanical support or heart transplantation. Coordinated care from a multidisciplinary team is key to improving outcomes.
Developed by EPG Health for Medthority, independently of any sponsor.
Related news and insights
Guidelines
of interest
are looking at
saved
next event