SABCS 2021 – HER2+ breast cancer update
In this focus article covering a San Antonio Breast Cancer Symposium (SABCS) 2021 Spotlight Session on novel therapies in HER2+ breast cancer, discover:
- Clinical trial updates
- How most HER2+ patients will be candidates for multiple lines of systemic therapy
- Updates on tyrosine kinase inhibitors (TKIs)
- Novel HER2+ treatments
Novel HER2+ Therapies and Clinical Updates
HER2+ breast cancer clinical results
Dr Priyanka Sharma University of Kansas Medical Center opened the spotlight session on HER2-positive breast cancer, presenting three abstracts on optimising the use of HER2 therapies in metastatic breast cancer (mBC).
Results from the DESTINY-Breast03 study with trastuzumab deruxtecan (T-DXd) has led to a practice-changing 72% improvement in progression-free survival (PFS) compared to trastuzumab emtansine (TDM-1)1.
Expression of HER2 is continuous, from HER2+ to around 45-50%, which are HER2-low. The DAISY study enrolled patients with advanced breast cancer regardless of HER2 status2 (n=186) but separated into three cohorts according to their HER2 expression. The primary analysis of confirmed best objective response (BOR) after 15.6 months follow-up was 70.6% in HER2+ (over-expressing), 37.5% in HER2-low, and 29.7% in HER2-non-detected patients. The median PFS (months) in HER2+ was 11.1, 6.7 in HER2-low, and 4.2 in HER2-non-detected.
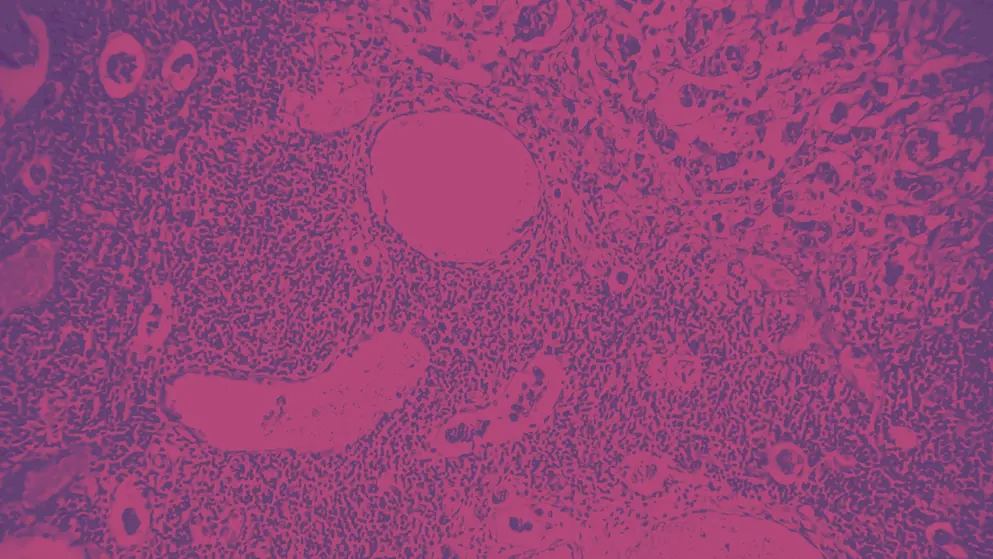
Dr Sharma also discussed the challenges around the reproducibility and sensitivity of immunohistochemical testing for HER2, and noted that more studies in this area are required3.
Results from the SOPHIA comparator study4 of margetuximab (M) and chemotherapy (CTX) versus trastuzumab (T) and CTX show a 24% risk reduction of disease progression with M. PFS was 5.8 months following M+CTX, and 4.9 months following T+CTX, although the median overall survival (OS) was not significantly different. While the subgroups are small, there is a suggestion that the advantages of either M+CTX or T+CTX may be due to allelic variants. We await the results from the ongoing MARGOT study, examining the efficacy of M and T with neoadjuvant therapies.
TKI results in HER2+ breast cancer
Dr Cristina Saura from Vall d’Hebron University presented updates in the treatment of HER2+ breast cancer with tyrosine kinase inhibitors (TKIs). The I-SPY 2 trial5 evaluated the safety and efficacy of tucatinib (300mg twice daily) when added to paclitaxel, pertuzumab and trastuzumab, in HER2+ stage II/III breast cancer. The efficacy data showed that following 12 weeks of therapy, 86% of patients had a greater than 80% reduction in tumour volume. However, following the enrolment of 20 patients, a safety analysis was conducted, and the tucatinib arm was suspended due to an unacceptable level of adverse events (AEs), despite reductions in tucatinib dose. Future studies of tucatinib will assess the AE profile using other antibody-drug conjugates (ADCs) to find a balance between its efficacy and reducing its toxicity.
The PHEDRA trial6 evaluated the safety and efficacy of pyrotinib (400mg daily) in combination with trastuzumab and docetaxel in Chinese patients with HER2+ early or locally advanced breast cancer (n=355). Pyrotinib is an irreversible pan-HER TKI targeting EGFR, HER2, and HER4. Compared to placebo, the addition of pyrotinib led to a statistically significant increase in total pathologic complete response (tpCR) from 22% to 41%, which was clinically meaningful. While adverse events were recorded in 75% of patients in the pyrotinib group, the safety profile was considered acceptable and manageable, leading to a high compliance rate. The results supported the use of pyrotinib, trastuzumab and docetaxel as a new neoadjuvant treatment option for HER2+ breast cancer patients. Future studies will assess the efficacy and toxicity of pyrotinib against standard of care therapies globally.
Finally, Dr Saura presented in vitro data from an abstract submitted by Veeraraghavan et al., who found that the mechanisms of resistance to tucatinib in two cell lines were associated with EGFR amplification which can be overcome by a complete blockade of HER receptors7. These preliminary data support the rationale to use EGFR inhibitors or pan HER inhibitors in response to tucatinib resistance. The limitations in this preliminary data may be overcome by repeating the research in other cell lines and in vivo models. Elucidating whether EGFR amplification only occurs in acquired resistance or whether there are intrinsic resistances to tucatinib through this mechanism need to be addressed through further translational research.
Novel therapies in HER2+ breast cancer
Dr Jo Chien presented data on novel therapies for HER2+ breast cancer. ARX788 is a fully humanised anti-HER2 monoclonal antibody, using a unique non-natural amino acid-enabled conjugation with AS269 drug linker, which is stable and has a relatively long half-life. In a phase I trial of 69 patients with HER2+ metastatic breast cancer, ARX788 showed promising efficacy of 66% objective response rate (ORR) in a post-trastuzumab, post-HER TKI setting. Drug-related high-grade AEs were low, which may be due to low levels of premature payload release. High rates of low grade ocular and pulmonary toxicity were seen8. A global phase 2 ARX788 monotherapy trial in patients post T-DM1, T-DXd, or tucatinib therapy is ongoing.
Dr Chien also presented data from the phase 3 PHENIX trial9 (n=274) on the safety and efficacy of pyrotinib in combination with capecitabine. The interim analysis showed that the addition of pyrotinib to capecitabine significantly prolonged PFS to 11.1 months compared to 4.1 months in the placebo/capecitabine arm. The patients on placebo/capecitabine (n=71) who crossed over to pyrotinib monotherapy at the time of progression had an ORR of 38%, with a PFS of 5.5 months. The rates of grade 3 or higher diarrhoea was comparable to other irreversible pan-HER2 TKI’s. The results from this trial were difficult to interpret in real-world terms due to the limited availability of HER2 therapies in China, meaning that the control arm was non-standard. However, the presenter highlighted the importance of developing drugs such as pyrotinib to improve access and outcomes globally.
The third abstract presented by Dr Chien discussed results from the SOLTI-1303 PATRICIA phase 2 study10. Patients with ER-/HER2+ mBC treated with palbociclib (CDK 4/6 inhibitor) and trastuzumab (n=15) had a low PFS rate at six months. Patients with ER+/HER2+ who received palbociclib/trastuzumab (n=28) with or without letrozole (n=28) had a comparable PFS at six months. Overall survival was longer in ER+ patients compared to ER-.
Following PAM50 analysis, 39% of patients had luminal A or B subtypes, resulting in a statistically significant improvement in PFS of 10.6 months versus 4.2 months in non-luminal subtypes. Overall survival in patients with luminal A or B subtypes was 38.6 versus 26.1 months, but this was not statistically significant. An extension to this study (Cohort C) is ongoing to determine whether luminal subtypes can predict the benefit of palbociclib in HER2+ patients. Patients with HR+/HER2+ mBC (n=232) PAM50 luminal tumours have been randomised to receive palbociclib + trastuzumab + endocrine therapy versus physicians’ choice of chemotherapy; we await the results.
As we enter a new era for HER2+ breast cancer, novel therapies will undoubtedly prolong PFS. However, there is also the risk of serious toxicity. Genomic and proteomic stratification of patients is needed to tailor individual therapies to individual patients, influenced by tumour biology, toxicity profiles, central nervous system effects, and access.
Join Professor Nadia Harbeck for an engaging discussion of all the top highlights from SABCS 2021, a deeper dive into HER2+ breast cancer, and advances in using TKIs in this video interview.
References
- Hurvitz S et al. Trastuzumab deruxtecan (T-DXd; DS-8201a) vs. trastuzumab emtansine (T-DM1) in patients (pts) with HER2+ metastatic breast cancer (mBC): subgroup analyses from the randomized phase 3 study DESTINY-Breast03. San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract GS3-01.
- Diéras V et al. Trastuzumab deruxtecan (T-DXd) for advanced breast cancer patients (ABC), regardless of HER2 status: A phase II study with biomarkers analysis (DAISY). Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-02.
- Lambein K, Van Bockstal M, Vandemaele L, Geenen S, Rottiers I, Nuyts A, Matthys B, Praet M, Denys H, Libbrecht L. Distinguishing score 0 from score 1+ in HER2 immunohistochemistry-negative breast cancer: clinical and pathobiological relevance. Am J Clin Pathol. 2013 Oct;140(4):561-6. doi: 10.1309/AJCP4A7KTAYHZSOE
- Rugo et al. Phase 3 SOPHIA study of margetuximab (M) + chemotherapy (CTX) vs trastuzumab (T) + CTX in patients (pts) with HER2+ metastatic breast cancer (MBC) after prior anti-HER2 therapies: Final overall survival (OS) analysis. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-01.
- Potter et al. Evaluation of Tucatinib + (paclitaxel + pertuzumab + trastuzumab) followed by AC in high-risk HER2 positive (HER2+) stage II/III breast cancer: Results from the I-SPY 2 trial. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-07.
- Wu et al. Pyrotinib in combination with trastuzumab and docetaxel as neoadjuvant treatment for HER2-positive early or locally advanced breast cancer (PHEDRA): A randomized, double-blind, mutlicenter, phase 3 study. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-08.
- Veeraraghavan et al. Acquired resistance to tucatinib is associated with EGFR amplification in HER2+ breast cancer (BC) models and can be overcome by a more complete blockade of HER receptor layer. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-06.
- Zhang J et al. Safety and anti-tumor activity of ARX788 in HER2-positive metastatic breast cancer patients whose disease is resistant/refractory to HER2 targeted agents (trastuzumab, ADCs, TKIs, and bispecific antibodies): ACE-Breast-01 trial results. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-04.
- Jiang Z et al. Overall survival (OS) results from the phase III PHENIX trial of HER2+ metastatic breast cancer treated with pyrotinib plus capecitabine. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-05.
- Ciruelos E et al. Palbociclib and trastuzumab for HER2-positive metastatic breast cancer (SOLTI-1303 PATRICIA): Final results from cohort A and B, prospective, open-label, multicenter phase II study. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD8-03.
of interest
are looking at
saved
next event
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
