SABCS 2021 – Brain Metastases: Managing LMD/Targeting HER2
In this topical article covering a San Antonio Breast Cancer Symposium (SABCS) 2021 Spotlight Session on HER2+ breast cancer and brain metastases, explore:
- Managing and targeting brain metastases
- Promising results for T-DXd in the CNS
- Call for patients with brain metastases to be included in clinical trials
- How genomics should be a part of the pathway of care using a validated framework
HER2+ and Brain Metastases
Treating brain metastases in HER2+ breast cancer
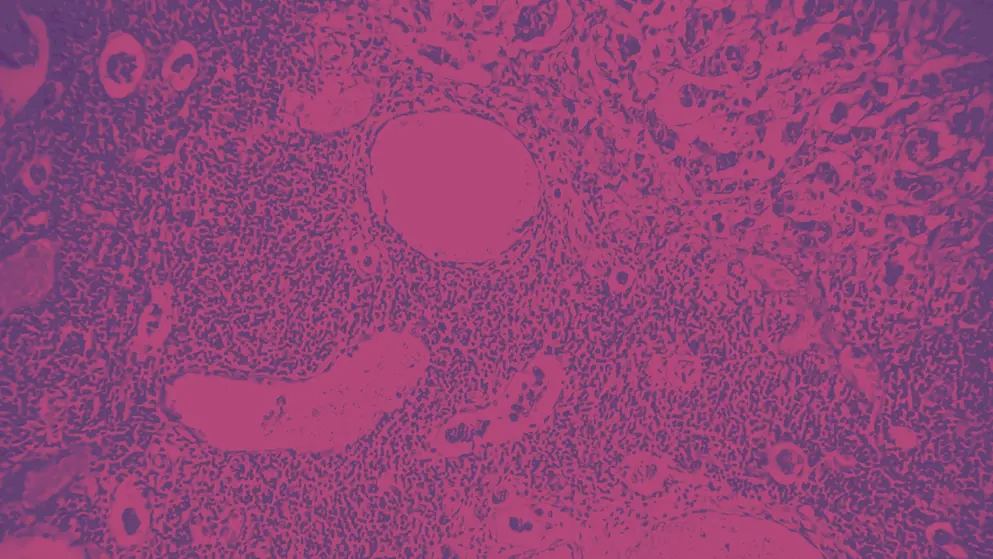
A high percentage of patients with HER2+ advanced breast cancer (BC) develop brain metastases (BM), and historically survival is poor. A SABCS 2021 spotlight session dedicated to managing and targeting leptomeningeal disease (LMD) in HER2+ breast cancer was kicked off by Dr Eudocia Lee from the Dana-Farber Institute, Boston.
The session began with updated results from the HER2CLIMB study1,2 showing a median overall survival (OS) of 10 months, following extended treatment with tucatinib combined with trastuzumab and capecitabine, with a clinically meaningful benefit in central nervous system progression free survival (CNS-PFS), consistent with the primary analysis2. This was the first prospective evidence of clinical benefit with a systemic regimen for HER2+ LMD.
Dr Patricia Steeg from the National Cancer Institute, Maryland, presented results which characterised the efficacy of trastuzumab and deruxtecan (T-DXd) in the CNS of 16 patients with HER2+ BMs3. Ten patients showed a partial response (PR), 6 of whom had progressive or unstable disease at baseline. The overall intracranial clinical benefit rate (complete response, PR or stable disease) was 75%, including 89% (8/9) of those with progressive or untreated BMs at baseline. These data suggest that T-DXd has intracranial efficacy against HER2+ BMs.
Encouraging preliminary results from the DEBBRAH4 phase 2 study of T-DXd in HER2+ and HER2-low-expressing advanced breast cancer patients with a history of BM or leptomeningeal carcinomatosis (LMC) were also presented by Dr Steeg. The primary endpoint of PFS at 16 weeks was reached in 75% of patients with HER2+ non-progressing BM, and CNS objective response rate (ORR) in 55.6% of those with progressing BMs. These were small cohorts, who were highly ER+, and not indicative of most HER2+ cohorts, therefore this study requires further follow-up.
Final discussions in the first part of the session highlighted the need to include patients with treated or stable BMs in clinical trials, rather than excluding them, in order to develop effective treatment options specifically for this group of patients.
Genomic profiling of brain metastases in HER2+ breast cancer
Research presented by Dr Athina Giannoudis5 suggests that BMs may be successfully treated with immune checkpoint and poly adenosine diphosphate-ribose polymerase (PARP) inhibitors, following analysis of their genomic landscape. Results showed that PD-L1 alterations were detected in 39% of BMs, and Programmed death-ligand 1 (PD-L1) protein expression was 27% in ER+/HER2+ and 57% ER-/HER2+ patients. These data reinforce the importance of acquiring BM material and cerebrospinal fluid for comprehensive genomic profiling.
Dr Fabrice André from the Université Paris-Saclay received the AACR outstanding investigator award for BC research. Using real-time genomic analysis of cancer biopsies (SAFIR02-BREAST)6, he showed that genomic analysis improves the outcome of patients with metastatic breast cancer if they carry alterations classified as ESMO Scale for Clinical Actionability of molecular Targets I/II (ESCAT I/II).
In this study, patients with metastatic HER2-non-overexpressing BC (n=1,462) underwent genomic profiling. After 6 to 8 rounds of chemotherapy (CT), those with genomic alterations were randomised to either targeted therapies matched to genomics or maintenance CT. The median progression-free survival (PFS) improved from two months to nine months when patients received targeted therapy matched to their genomic alteration, compared to maintenance CT (hazard ratio [HR]=0.41). However, results in the intent-to-treat population were not statistically significant (2 months to 5.5 months, HR 0.77, p=0.109). Subgroup analysis revealed that the level of ESCAT classification was highly predictive for the benefit of targeted therapy. The study concluded that it is imperative for all patients to have access to genomic analyses and be offered genomic testing to detect ESCAT I/II alterations. Targeted therapy matched to a genomic alteration should not be administered beyond ESCAT II.
Dr André stated that “These findings suggest that genomics should be a part of the pathway of care, but it has no impact if the results are not interpreted using a validated framework of actionability of the gene alterations identified.”
Finally, from the HER2 heterogeneity forum, Dr Aleix Prat from the Medical Oncology Department, Barcelona, Spain, described the molecular heterogeneity in HER2+ breast cancer and whether outcomes can be predicted. Even within patients designated as having very high levels of HER2+, there can be a twelve-fold difference in their mRNA levels. Tumour infiltrating lymphocytes (TILs) and immune genes may predict the pathologic complete response in HER2+ disease but do not always predict survival outcomes. Biopsies taken during treatment may increase individual heterogeneity but provide a better prognosis of the patient’s outcome at surgery and during follow-up. A combination of biological variables is needed to better predict outcomes, and they should be included in all future clinical trials.
Join us for our next SABCS 2021 highlight article which explores HER2+ breast cancer novel therapies and clinical results.
References
- Lin NU et al. Updated results of tucatinib vs placebo added to trastuzumab and capecitabine for patients with previously treated HER2-positive metastatic breast cancer with brain metastases (HER2CLIMB). Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD4-04.
- Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N Engl J Med. 2020 Feb 13;382(7):597-609. DOI:10.1056/NEJMoa1914609
- Kabraji S et al. Preclinical and clinical efficacy of trastuzumab deruxtecan in breast cancer brain metastases (BCBM). Presented at the San Antonio Breast Cancer Symposium, 7-10 December 2021. Abstract PD4-05.
- Vaz Batista M et al. Trastuzumab deruxtecan in patients with HER2[+] or HER2-low-expressing advanced breast cancer and central nervous system involvement: Preliminary results from the DEBBRAH phase 2 study. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD4-06.
- Giannoudis A et al. Comprehensive assessment of the genomic landscape of breast cancer brain metastases reveals targetable alterations and genomic signatures relevant to immune- checkpoint and PARP inhibitors. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract PD4-09.
- André F et al. Clinical utility of molecular tumor profiling: Results from the randomized trial SAFIR02-BREAST. Presented at the San Antonio Breast Cancer Symposium, 7–10 December 2021. Abstract GS1-10.
of interest
are looking at
saved
next event
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
