ECCMID 2022 Congress Highlights
ECCMID 2022 Congress highlights
Stay up to date with the latest in infectious diseases from the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022, covering:
- The impact of the COVID-19 pandemic on infectious disease research, surveillance and treatment
- Other infectious respiratory diseases
- A focus on respiratory syncytial virus (RSV) infections
In this section
Day One – Impact of COVID-19 on infectious disease
By Heather Mason
The 32nd European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) kicked off in a hybrid format, both online and on site, in Lisbon, Portugal on April 23rd. In his welcome speech, the President of host society ESCMID, Maurizio Sanguinetti, acknowledged the changes that have occurred since the last ECCMID meeting in 2019. Notably, that COVID-19 was then unknown, and that it now represents the subject of over 20% of all abstracts submitted to this meeting.
The COVID-19 pandemic has served to highlight several aspects of infectious disease management. These include the central position of laboratory medicine in healthcare systems, with the expansion of rapid testing capacity and test refinement; biobanking to tackle the multifactorial aspects of disease; machine learning to integrate clinical and laboratory data; collaboration towards national surveillance systems, and syndromic diagnostics (such as respiratory) to prevent patient isolation and decrease antibiotic use. Each of these topics will be covered in more detail during the coming days of the congress.
Abstracts on COVID-19 made up more than one fifth of submissions to this year’s ECCMID
While the programme covers a broad range of topics, the COVID-19 pandemic has also affected the incidence of other respiratory viruses, largely due to the implementation of public health measures. Several poster presentations showed that the usual winter peaks of respiratory syncytial virus (RSV) infections and influenza disappeared during the winter of 2020-2021, but that RSV reappeared during the summer months, perhaps due to the mitigation of COVID-19 health measures1-3.
COVID treatment insights – what have we learnt?
Davide Bavaro presented data on 394 patients with COVID-19 who either received home corticosteroid therapy (n = 125), or those that did not (n = 269)4. While the period between symptom onset and hospitalisation was delayed in those who had corticosteroids, they experienced higher rates of acute respiratory failure requiring oxygen (92% vs 67% P<0.001) and a trend towards increased mortality at day 30 (10% vs 6% P=0.089). He concluded that corticosteroids should be avoided, at least in the early disease phase. This advice was substantiated by Ana Motos Galera, who presented data from an observational study conducted in patients who had been in the ICU for two days or more, and who had not previously received corticosteroids5. The primary outcome of all-cause mortality revealed that in hospital mortality was similar between those who received corticosteroids and those who did not. However, multivariate analysis revealed that in those under 60 years of age, with lower baseline disease severity, or with a low inflammatory response (C-reactive protein, lymphocyte count) at ICU admission, no benefit was observed. In fact, early administration of corticosteroids (<7 days) was associated with a higher risk of mortality (hazard ratio 1.27, 95% confidence interval 1.07-1.50), a higher risk of nosocomial bacterial pneumonia, hyperglycaemia, and haemorrhage. This study concluded that not only do corticosteroids fail to provide a benefit, but they may also, in fact, be harmful in certain populations.
While corticosteroids appear to confer little benefit, and potential harm, when used for COVID-19, other treatments are proving more effective at preventing hospitalisation and death in clinical trials
Phillip Monk presented data from a Phase II trial on the daily use of a nebulised formulation of interferon-β (IFN-β) (n = 48), or placebo (n = 50), in adult patients hospitalised with COVID-196. At the end of the 14-day dosing period, 39% on placebo progressed to severe disease (two of whom died) compared to 17% of patients receiving IFN-β (none died). These results have prompted the initiation of the Phase III SPRINTER trial, focusing on patients receiving supplemental oxygen.
The early initiation of anakinra has also shown to increase the rate of COVID-19 resolution, and decreased the incidence of long COVID, according to the results of the randomised, double blind SAVE-MORE study7, presented by Evangelos Giamarellos-Bourboulis. The odds ratio for worse outcome under anakinra compared to placebo was 0.40 on day 60 and 0.50 on day 90. Anakinra treatment was also associated with a significant survival benefit of 5.7% compared to 10.6% in the placebo group.
Hugh Montgomery presented primary data analysis from the TACKLE (NCT04723394) Phase III double-blind, placebo-controlled trial of AZD7442, comprising two fully human, extended half-life, neutralising antibodies, in non-hospitalised patients with mild to moderate COVID-198. A one-time intramuscular injection of AZD7442 (n = 452) or placebo (n = 451) was given ≤7 days from symptom onset. The primary endpoint was severe COVID-19 or all-cause mortality to day 29. In the primary efficacy analysis AZD7442 reduced the risk of developing severe COVID-19, or death, by 50%, increasing to 67% if given before 5 days, and 88% if given ≤3 days from symptom onset. Follow up in vitro analysis suggests that AZD7442 has no decrease in efficacy for the Omicron variant.
The data on the epidemiology, treatment and vaccination strategies of SARS-CoV-2, and its comparison to influenza and RSV, have also highlighted how the treatment of respiratory viruses are contributing to multi-drug antibiotic resistance. This is an exciting subject that will be covered in tomorrow’s highlights article.
Day Two – SARS-CoV-2 and other respiratory viruses
By Heather Mason
Are there positives to come out of the COVID-19 pandemic?
What positive outcome could have possibly come out of the COVID-19 pandemic? Essentially, the revolution of respiratory virus testing. Even as recently as 2019, the capacity, turnaround time, and specificity of testing were a challenge. With the pandemic, laboratories and industry have collaborated to provide more accurate and rapid testing, with increased testing capacity for a wide range of respiratory viruses.
Despite extensive morbidity and mortality, the COVID-19 pandemic has spurred advances in multiple areas of infectious disease care, particularly rapid testing for respiratory infections
An integrated symposium called for an end to prescribing antibiotics for viral respiratory infections, noting that they are contributing to antibiotic resistance. Louis Bont presented data where an expert panel diagnosed paediatric patients between 2 and 60 months of age with a bacterial, viral or unknown cause respiratory infection, based on presenting symptoms and follow-up data9. Their responses were compared to results from genomic data, which revealed that most respiratory infections were of viral origin, for which the study showed a high percentage of clinicians would have prescribed antibiotics. The future of diagnosing and successfully treating paediatric respiratory viruses lies with bedside multiplex polymerase chain reaction (PCR) diagnosis.
Co-existence of SARS-CoV-2 and respiratory viruses
Yonat Shemer presented data on the prevalence of common infectious diseases after COVID-19 vaccination and the easing of mitigation measures10. Growth rates of respiratory infections in the community were examined over time, detected by real-time PCR testing. Circulating adenovirus, human coronavirus, and rhinovirus levels did not change during 2020-2021, while influenza A, B, RSV, and human metapneumovirus (HMPV) disappeared. It is unknown why certain viruses disappeared while others did not. This trend has also been seen globally.
Children aged 0 to 3 years had significantly increased rates of respiratory and gastrointestinal infection diagnoses following the easing of restrictions. During the lockdown, children had been restricted to interactions with family, and it is feared that as the world comes back into our ‘new normal’, it is likely that we will see increased susceptibility to bronchiolitis in 0 to 2 year-olds due to lack of immunity.
The expanded technology for virus detection has provided essential epidemiological data and will also offer interesting insights into remerging infection as global COVID-19 cases decline. Catherine Moore from Public Health Wales reflected on her experience of the H1N1 pandemic, which saw the circulation of other respiratory viruses, and co-infections lead to increased death rates11. Their COVID-19 testing regimen was added to their existing screening for other seasonal viruses. The overall increase in testing saw detection of RSV and parainfluenza cases in children that would not have previously been part of the differential diagnoses. They also found that cases of dual SARS-CoV-2 and RSV infections did not result in an increase in COVID-19 severity. Due to the low numbers of influenza cases, there is no clear signal whether co-infection between influenza and COVID-19 leads to an increase in disease severity. All seasonal viruses still remain, and as cases of COVID-19 decrease, the next few months will show how COVID-19 fits into the overall epidemiology of respiratory infections. The COVID-19 pandemic has highlighted the fact that we do not look hard enough for seasonal viruses. Dr Moore reiterated the fears expressed by Dr Shemer that coming back into the ‘new normal’, it will be the paediatric population born during mitigation measures which will be most severely affected as their maternal immunity wanes. Moving towards symptomatic hospital multiplex PCR testing will give better quality data on which seasonal viruses are circulating, and this will enable monitoring of co-existing viral infections. In addition, providing a definitive diagnosis for children with milder respiratory symptoms can help to prevent the over-prescription of antibiotics.
Some common respiratory infections, such as influenza and RSV, saw reduced incidence during the COVID-19 pandemic; others, such as adenovirus and rhinovirus, did not
An interesting presentation by Cristian Perez Corrales highlighted the challenges of testing procedures in low- and middle-income settings, where resources are limited12. He describes analysis from a multiplex PCR assay of 49 paediatric patients who had tested positive for SARS-CoV-2, 43% of whom also had a co-infection. In blind specimens (n = 58), 17% were SARS-CoV-2 positive, 57% had other viruses, 14% had co-infections, and no virus was detected in 21%. The multiplex analysis mitigated the need for further testing in 21% of cases, reducing cost and turnaround time.
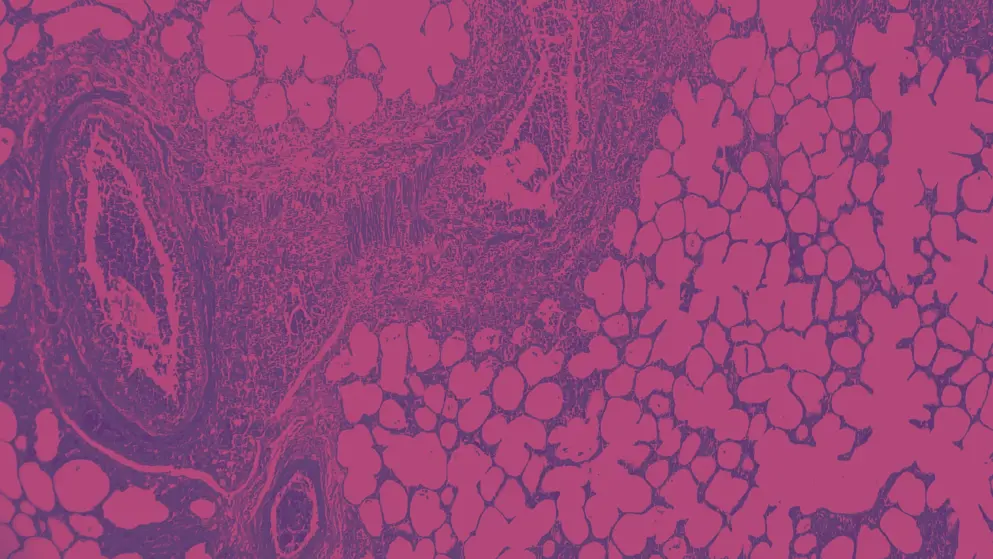
At the end of this session9, an interesting issue was raised. As pre-pandemic seasonal respiratory viruses were not routinely monitored, the advances in multiplex PCR analysis now enable the simultaneous screening of multiple viruses. It would be interesting to determine whether the multisystem inflammatory syndrome seen in children is related to co-infections with any of these other viruses that have not previously been diagnosed. Other respiratory viruses in hospital settings Intensive care unit (ICU) patients are one of the most vulnerable groups of patients because of their severity of illness. Hence it is increasingly being recognised that ICU patients are vulnerable to acquiring healthcare-associated infections that may, in part, be caused by viruses. Clinicians should be aware of respiratory viral infections other than COVID-19, which account for between 15 and 20% of all ICU admissions due to community-acquired pneumonia; 10% of these are due to RSV. Charles Eduard Luyt highlighted that reactivation of latent herpes viruses occurs frequently, due to critical illness-induced impairment of cellular immunity13. While a higher HSV viral load is related to poor outcomes in critically ill patients, the rate of reactivation of HSV is less with COVID-19 than that seen with influenza. In these cases, prophylactic acyclovir has not significantly affected outcomes. Tomorrow, we look further into the burden of RSV in the paediatric population and where artificial intelligence may become invaluable in the management of infectious diseases.
Day Three – Focus on respiratory syncytial virus
By Heather Mason
Hepatitis of unknown aetiology in children – Late-breaking session
A late-breaking session in today’s proceedings was co-organised by the EU commission in order to discuss the mystery strain of hepatitis of unknown aetiology affecting children14,15. The number of RSV-related deaths in the US is higher in those under one year old and over 50 years, with a peak of deaths in those aged 80–89 years. In children younger than five years with RSV, 58.6% of deaths are directly related to RSV.
Annual attack rates can be higher in long term care facilities, and the disease burden is expected to increase as the population increases in age. While RSV has fewer infections than influenza, RSV appears with more regular incidence each year. The effect of comorbidities is higher with RSV than influenza in age-matched patients over 65 years, as measured by the Charlson comorbidity index.
Seasonal hospital admission attributable to RSV is 71/100,000 for the 65–74 age group but 251/100,000 for those over 75 years of age. The burden of RSV in community-dwelling older adults in Europe was investigated in the RESCEU study16. This study found that atypical and delayed presentation, complex multimorbidities, an ageing immune system, polypharmacy, prolonged hospital stay and residing in long-term care facilities all increase the mortality risk of RSV in older adults.
RSV risk is heightened in the young and the elderly, with comorbidities playing an increased role in older patients
Patients with chronic obstructive pulmonary disease, congestive heart failure, haematologic malignancies, stroke, and chronic kidney disease all see increased risk of hospitalisation from RSV infection. Cardiovascular disease can also be induced by viruses such as RSV, influenza, urinary tract infections and shingles. This is related to the acute inflammatory response, plaque destabilisation and thrombogenesis, triggering acute myocardial infarction increasing mortality and health care utilisation.
The incidence ratio for acute myocardial infarction within seven days of an RSV infection is 3.5, slightly lower than influenza but still important. RSV is also a risk for immunocompromised patients. There are efforts underway to stratify and understand the contributing risk factors leading to severe disease in this population17.
A final scenario discussed by Dr Blasi was the role of RSV infection in lung transplant patients. RSV infection is associated with an increased risk of allograft rejection and death in these patients. If there is a decline of 10% in forced expiratory volume (FEV1), there is an increased risk for mortality.
RSV infection can exacerbate existing health conditions, such as cardiovascular disease
Elen Vink presented data on the aetiology, trends and diagnostics for acute respiratory infections, the leading cause of infectious disease worldwide and the fourth most common cause of death18. The aetiology of acute respiratory infections differs by age, geography, comorbidities, and history of exposure to environmental factors. A large proportion of respiratory infection cases do not have an identified pathogen.
Aetiology is changing. Recent trends show that pneumococcal pneumonia has decreased, and antimicrobial resistance has increased. The impact of the COVID-19 pandemic has led to an increased awareness of viral infection. Increased funding for testing and improved testing infrastructure, have, in turn, led to a decrease in testing for other viruses and also a disruption in routine vaccination. Public health measures have also changed the seasonal circulation of other viruses.
Viral co-infection during the first 18 months of the pandemic was rare (2%) and caused by various viruses, none of which increased the severity of COVID-19. No co-infection was detected after mid-May 2020.
The COVID-19 pandemic has caused major changes in the observed incidence of other respiratory infections, including RSV
Dr Vink presented data from the ISARIC WHO CCP-UK prospective cohort study19, which was the first large study of co-infection in COVID-19 patients (n > 240,000), across 36 sites, collecting data up to 28 days post-discharge. It was also the first study that accounted for seasonality. The limitations were that the low number of co-infected patients did not allow for significance to be determined, and most data was collected in the first wave of COVID-19, the landscape having since changed.
Further prospective data is required on co-infections now that public health restrictions have eased, and patients should be sampled at admission. Ongoing surveillance of respiratory viruses in circulation is also needed to assess the dynamics and seasonality of respiratory infections.
Changing respiratory infection dynamics will require careful observation and follow-up in affected patients
Angela Branche commented that the RSV burden in older adults is still underestimated, as symptoms could be related to many other respiratory viruses, testing is not routine, and there is little motivation to give a definitive diagnosis due to the lack of effective therapies20. A study by Falsey et al. found that 7.4% of elderly patients with influenza were positive for RSV, increasing to 8.7% of over 75-year-olds and 12.5% of elderly patients requiring hospitalisation21. The duration of symptoms for acute respiratory illness (ARI) caused by RSV is wide (9.5–19.0 days), and even longer for older and high-risk adults.
Dr Branche also presented data from a clinical study conducted in France22, which analysed patient outcomes following RSV infections with influenza-like illness (n = 1452). They found that pneumonia was more likely to occur in patients with RSV (44%; 23/53) than in patients who were RSV-negative (26%; 362/1393) (P=0.006), or with influenza virus infection.
A report from Prill et al. showed that younger adults from 20–69 years account for a substantial number of deaths due to RSV, but these are not always listed as the cause of death and therefore may be underestimated23.
One year survival rates in patients with pneumonia due to RSV were poorer among those with baseline chronic heart failure (CHF) or CHF exacerbation compared to those without cardiac morbidity at baseline. No significant differences in survival were observed for those with COPD, chronic bronchitis, or emphysema.
Dr Branche also highlighted that a change in functional status is more important to the patients. At 6-months post-discharge, 32% reported poor functional outcomes compared to pre-hospitalisation. When stratified by pre-hospitalisation living situations, those in care fared worse.
Conclusions from this symposium on RSV include:
- RSV in adults is an under-recognised cause of deterioration in health, particularly in frail elderly patients
- RSV is the most common single cause of respiratory hospitalisation in infants and the second-largest cause of lower respiratory infection mortality worldwide
- As testing is not routine, the real burden of RSV may be much higher
- Specific vaccination programmes and antiviral therapy may benefit those at high risk
Day Four – Respiratory syncytial virus burden in infants
By Heather Mason
This year’s ECCMID draws to a close
As we reach the end of this ECCMID congress, we will conclude our coverage with the burden of respiratory syncytial virus (RSV) infection in infants and the final flash mini-oral session on respiratory viruses.
The burden of RSV in infants
Virtually all infants are infected with RSV in the first two years of life, which can lead to severe bronchiolitis and pneumonia. One in five infants infected with RSV will require outpatient care, and one in fifty is hospitalised within the first year of life, an event linked to a 39% increase in recurrent wheezing in adolescence24. There is a current lack of approved prophylaxis other than palivizumab which is only approved for high-risk and preterm infants25.
Paulo Manzoni reviewed the trends of RSV during the COVID-19 pandemic26. In Piedmont, Italy, a 76% decrease in paediatric hospital admissions related to infectious diseases was found during the pandemic, as well as an 84% decrease in acute bronchiolitis, trends reflected across the rest of Europe. This drop in bronchiolitis cases was not due to the reduction in the circulation of RSV alone. Other enveloped virus infections were significantly reduced, while non-enveloped viruses such as rhinovirus, adenovirus, and bocavirus remained at typical infection rates. Data from 244 children hospitalised for COVID-19 found co-infections in 28.3% of cases (viral n = 45; bacterial n = 32). Of these, 11.6% had multiple infections. In a separate study, COVID-19 and RSV (n = 6) co-infections were always mild and uncomplicated.
Following the relaxation of social distancing measures, there has been a surge of RSV infections, an alteration of historical seasonality, and increased severity during peak phases. Explanations for the surge in RSV may relate to the infant population naïve to RSV after 12–18 months of lockdown, potentially causing reduced immune defences, less viral clearance, increased severity, and older age of infection. Also, pregnant mothers have had lower exposure to RSV, meaning that fewer maternal antibodies are passed to the infants. Experts predict that increased RSV incidence in older infants will continue for one or two following seasons.
RSV incidence has changed in light of public health measures and may continue to affect infants more severely in the near future
Heather Zar presented new data on the persistent burden of RSV and future interventions27. Around 79% of infants hospitalised with RSV are born healthy with no comorbidities (unlike the adult population), and RSV accounts for 2% of all infant deaths <6 months of age in developing countries. The Drakenstein birth cohort longitudinal study looked at the acute and persistent burden of RSV28. The study found that children with a first RSV lower respiratory tract infection (LRTI) were three times more likely to develop recurrent LRTI than those with non-RSV LRTI.
A meta-analysis study analysed the risk of RSV and subsequent wheezing and found that RSV LRTI and hospitalisation for all-cause LRTI were independently associated with recurrent wheezing. While RSV LRTI does not directly cause wheezing, it identifies at-risk children and is an important predictor of adult mortality.
Octavio Ramilo presented data on the immunopathogenesis of RSV in infants, noting that age and viral load are very important29. Fifty percent of hospitalised cases are under three months, and 70% are under six months of age. When clinical symptoms are compared across age groups, wheezing and fever were reduced in those under three months of age compared to 3–6 months or 6–24 months. Viral loads are higher in outpatients than in hospitalised patients, but the link between viral load and severity is unclear.
Mini-oral flash session – viral respiratory infections
Kate Beard presented data on integrating routine syndromic molecular point-of-care testing for respiratory viruses in an adult acute oncology unit30. The primary outcome was time to available results pre- and post-implementation, which was reduced from 5.8 to 1.9 hours. This decrease was mirrored by a corresponding reduction in length of hospital stay, time of radiology request to results, and importantly, the number of cases of hospital-acquired infections decreased from 20 cases pre-implementation to zero post-implementation. While the study had limitations, overall, there was an improvement in patient care following the implementation of their point-of-care testing.
Grace Chen Phillips presented safety and immunogenicity data from a randomised, observer blind, placebo-controlled, dose escalation phase I trial on an mRNA-based vaccine candidate (mRNA-1345) against RSV in adults 6579 years of age31. Participants were boosted with the same dose at 12 months. Treatment-related unsolicited adverse events within seven days of dosing were reported in 6.7% of mRNA-1345 recipients and 10.2% of placebo recipients. Unsolicited severe adverse events were reported in 2.9% of mRNA-1345 recipients but none in placebo recipients. All participants had neutralising antibodies (nAb) at baseline, suggesting prior exposure to RSV. mRNA-1345 boosted both RSV-A and RSV-B geometric mean titres. At one month, the geometric mean fold rise in nAbs was 9.8–16.9 for RSV-A and 5.3–12.3 for RSV-B. These results support the ongoing development of the mRNA 1345 vaccine in this population.
Despite the pandemic, vaccine development for preventing viral respiratory infections continues in multiple clinical trials
Results of a phase III trial of a recombinant, quadrivalent, hemagglutinin saponin adjuvanted nanoparticle influenza vaccine (Nanoflu) against vaccine homologous and antigenically drifted viruses was presented by Vivek Shinde32. It is widely appreciated that antigenic drift and a lack of induced T cell response is a limitation of current influenza vaccine strategies. In this non inferiority study, participants were stratified according to whether they received an influenza vaccine in the previous season, receiving either an approved influenza vaccine or Nanoflu (1:1). Nanoflu had a 24–66% higher wild-type HAI antibody response on all four homologous strains and a 34–46% increase against six drift strains compared to the approved vaccine. Nanoflu significantly increased the induction of double cytokine (at least two of interferon-𝛾, TNF-⍺, IL-2, or CD40L+) effector CD4+ T cells against homologous and drifted strains compared to the approved vaccine, and these remained elevated after one year.
Key conclusions from ECCMID 2022
- COVID-19 has shifted the landscape of other seasonal viruses, with RSV appearing outside of the winter season and other viruses mostly disappearing during the pandemic
- Viruses unaffected by COVID-19 include rhinovirus, adenovirus, parainfluenza, and other coronaviruses
- We wait to see the outcomes of the emerging crisis of hepatitis of unknown origin in the paediatric population
- The pandemic has resulted in an expansion of national testing infrastructures and technologies, enabling fast-track results
- As the world re-emerges from the COVID-19 pandemic, national diagnostic and permanent surveillance systems should now begin to include seasonal viruses as part of their future testing policy, including the start, duration, timing and intensity of viral outbreaks
- Machine Learning has the potential to improve the speed and quality of patient diagnostics and reduce antibiotic overprescribing
Expert Interview – Professor Antoni Torres
Watch as Professor Antoni Torres from the University of Barcelona gives an expert overview of important developments at ECCMID 2022. From COVID-19 to respiratory syncytial virus to pneumococcal disease, Professor Torres provides some of the latest research insights in this brief interview.
In this video, Professor Torres discusses:
- Learning more about and preventing COVID-19
- New vaccines and changing serotypes in pneumococcal disease
- Gram-negative bacteria and antibiotic resistance
- RSV symposium overview
- Importance of rapid testing for antiviral and antibacterial drug development
- Burden of RSV disease in adults
- Advances in diagnostic testing
References
- Bernet Sanchez A, Lopez Gonzalez E, Mormeneo Bayo S, Prats I, Belles Belles A, Aramburu Arnuelos J, et al. What happens with RSV? Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. P0042.
- Sebastião M, Fradique AR, Gata L, Rodrigues F. Respiratory syncytial virus (RSV) infection in children in the era of SARS-CoV-2. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. L0354.
- Torres A, Martinón-Torres F, Weber K, Cáceres A, Gutierrez C. Clinical burden of respiratory syncytial virus (RSV) and influenza in hospitalised adults: a retrospective IASIST analysis. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 23 April. LIsbon. P0026.
- Balena F, Pallara E, Vita ED, Lattanzio R, Iaco GD, Mariani MF, et al. Association of home corticosteroids therapy with COVID-19 disease severity and mortality. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. O0140.
- Motos A, Cillóniz C, Ceccato A, Fernández-Barat L, Gabarrús A, Bermejo J, et al. Benefit and harm of corticosteroids in large population of COVID-19 patients admitted to Spanish intensive care units. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. O0145.
- Monk P, Tear V, Brookes J, Batten T, Mankowski M, Gabbay F, et al. Effects of inhaled interferon-beta on hospitalised COVID-19 patients receiving supplemental oxygen. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. O0143.
- Giamarellos-Bourboulis E, Kotsaki A, Metallidis S, Papailiou A, Rapti A, Taddei E, et al. Long-term benefit of early anakinra treatment in COVID pneumonia at risk: results of the SAVE-MORE trial. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. O0144.
- Montgomery H, Hobbs R, Padilla F, Arbetter D, Templeton A, Seegobin S, et al. Efficacy and safety of intramuscular administration of AZD7442 (tixagevimab/cilgavimab) for early outpatient treatment of COVID-19: the TACKLE phase III trial. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. O0146.
- Bont L, Bogaert D, Tiemann C. Facing a 'new normal': co-existence of SARS-CoV-2 and respiratory viruses. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 24 April. Lisbon. IS17.
- Shemer Y. The trend prediction and prospectives on respiratory disease in the "Living with COVID-19" and "Post COVID-19" era. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 24 April. Lisbon. IS17
- Moore C. Support for Public Health Wales in the fight against SARS-CoV-2 and variants. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 24 April. Lisbon. IS17
- Perez Corrales C. Diagnostic stewardship for respiratory infections in a pediatric hospital: big challenge from single-virus mild infections to severe co-infections between SARS-CoV-2 and other respiratory viruses. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 24 April. Lisbon. IS17
- Luyt C. Respiratory virus infections in ICU patients besides SARS-CoV-2: what matters? Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 23 April. Lisbon. SY044
- Kantele A, Moran-Gilad J, Mougkou A, Chand M. Special session: hepatitis of unknown aetiology. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 25 April. Lisbon. S86.
- Blasi F. Incidence, severity and impact of RSV. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 25 April. Lisbon. IS36.
- Korsten K, Adriaenssens N, Coenen S, Butler C, Ravanfar B, Rutter H, et al. Burden of respiratory syncytial virus infection in community-dwelling older adults in Europe (RESCEU): an international prospective cohort study. Eur Respir J. 2021;57(4).
- Nam HH, Ison MG. Respiratory Syncytial Virus. Semin Respir Crit Care Med. 2021;42(6):788-799.
- Vink E. Multiplex testing and the detection of common respiratory pathogens. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 25 April. Lisbon. IS36.
- Russell CD, Fairfield CJ, Drake TM, Turtle L, Seaton RA, Wootton DG, et al. Co-infections, secondary infections, and antimicrobial use in patients hospitalised with COVID-19 during the first pandemic wave from the ISARIC WHO CCP-UK study: a multicentre, prospective cohort study. Lancet Microbe. 2021;2(8):e354-e365.
- Branche A. RSV and older adults: an underestimated pathology? Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 25 April. Lisbon. IS36.
- Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352(17):1749-1759.
- Loubet P, Lenzi N, Valette M, Foulongne V, Krivine A, Houhou N, et al. Clinical characteristics and outcome of respiratory syncytial virus infection among adults hospitalized with influenza-like illness in France. Clin Microbiol Infect. 2017;23(4):253-259.
- Prill MM, Langley GE, Winn A, Gerber SI. Respiratory syncytial virus-associated deaths in the United States according to death certificate data, 2005 to 2016. Health Sci Rep. 2021;4(4):e428.
- Smith DK, Seales S, Budzik C. Respiratory Syncytial Virus Bronchiolitis in Children. Am Fam Physician. 2017;95(2):94-99.
- Garegnani L, Styrmisdóttir L, Roson Rodriguez P, Escobar Liquitay CM, Esteban I, Franco JV. Palivizumab for preventing severe respiratory syncytial virus (RSV) infection in children. Cochrane Database Syst Rev. 2021;11(11):Cd013757.
- Manzoni P. Rethinking RSV epidemiology, past, present, and future. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 24 April. Lisbon. IS30.
- Zar H. Reimagining the acute and persistent burden of RSV in all infants. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 24 April. Lisbon. IS30.
- Zar HJ, Nduru P, Stadler JAM, Gray D, Barnett W, Lesosky M, et al. Early-life respiratory syncytial virus lower respiratory tract infection in a South African birth cohort: epidemiology and effect on lung health. The Lancet Global Health. 2020;8(10):e1316-e1325.
- Ramilo O. The immunopathogenesis of RSV and challenges in infant immunity. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 24 April. Lisbon. IS30.
- Beard K. Impact of integrating routine, syndromic molecular Point-of-Care testing for SARS-CoV-2 and other respiratory viruses into an acute oncology service. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 26 April. Lisbon. OF222.
- Chen Phillips G. Safety and immunogenicity of mRNA-1345, an mRNA-based vaccine against respiratory syncytial virus in older adultse. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 26 April. Lisbon. OF222.
- Shinde V. Long-term durability of antigen-specific polyfunctional CD4+ T cell responses against vaccine-homologous and antigenically drifted viruses: results of a phase III trial of a recombinant quadrivalent hemagglutinin saponin-adjuvanted nanoparticle influenza vaccine in older adults. Presented at the European Congress of Clinical Microbiology and Infectious Diseases 2022, 26 April. Lisbon. OF222.
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
Developed for Medthority by EPG Health. This content has been developed independently of the sponsors who have had no editorial input into the content. EPG Health received unrestricted educational funding from the sponsor in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.
