Managing High-Risk NMIBC
Transcript: EAU25: Expert reflection
Ashish Kamat, MD, MBBS, FACS
Interview recorded March 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
Whenever phase 1 data is presented at a large congress or conference like this, it sometimes loses the audience because it appears like it's very early. And I think what we should take home from this presentation is, yes, it is early, but it's a natural sort of evolution of the gene therapy drug delivery space. Again, this abstract had small numbers of patients, but we can draw from the fact that the agent has been used in uveal melanoma in the past. So there is proof of principle from other disease states, and you're clearly seeing activity in the light activated group of patients. So small number of patients, a clear signal that exists and I think having alternatives to actual viral delivery of therapy is critical because there are infrastructures in the world that can't support the existing viral drug delivery. And I think, again, early data, but it's encouraging and excited to see how they take it into phase 2 and further stages of development. It's really been great to see the progressive data coming out from the CG, and I use CG as a short-form agent. Oftentimes what happens is when you have more patients enrolled in a clinical trial, the efficacy numbers go down. But here, we're actually seeing them staying robust around 75-ish percent plus or minus. And I think it's really good to see that even the updated data has the bar at a higher level.
So clearly CG is one of the agents that we're all looking forward to, to seeing the mature data. And of course, we're hoping that eventually when this goes in front of regulatory bodies, if it gets approved, it is some therapy that's available for our patients and that we have more choices. So exciting data and looking forward to seeing what the next iteration brings. For many years, we've relied on BCG as being the backbone of treatment for patients with high-risk, non-muscle-invasive bladder cancer and justifiably so because BCG has an excellent response rate. In fact, in more contemporary series, that response rate has been the highest it's ever been. But clearly there are patients who do not respond to BCG and need an alternative. So combinations with systemic agents, especially checkpoint inhibitors, has been studied and some will be presented later this year. And of course, there's role for other combinations. And when we see the results of the DV, which is a targeted ADC, of course, and it is systemic, it's encouraging that it appears that the combination is better than single agent alone.
Now of course, when you look at any systemic drug, it has additional systemic toxicity. So we don't want to necessarily assume that if this ends up in a larger phase study showing a signal, it might be applicable for all patients. But then we have the target, and we do know from prior studies that there are subtypes of bladder cancer, especially micropapillary for example, that do not respond well to BCG, and you have a target now that could potentially target the therapeutic pathway in those patients. So I think this is a great piece of information for us to digest, see how we can use it in selected sub-populations. And as with all the treatments that are coming out, I think the key is going to be in personalized selection of the right therapy for the right patient. And having an ADC like this that has efficacy, we know that, and has a target that we can identify with IHC or genetic profiling, would actually really move the field forward if the toxicity profile is favorable for the patient. So I was really pleased to see this abstract and looking forward to seeing what they do in an expanded trial.
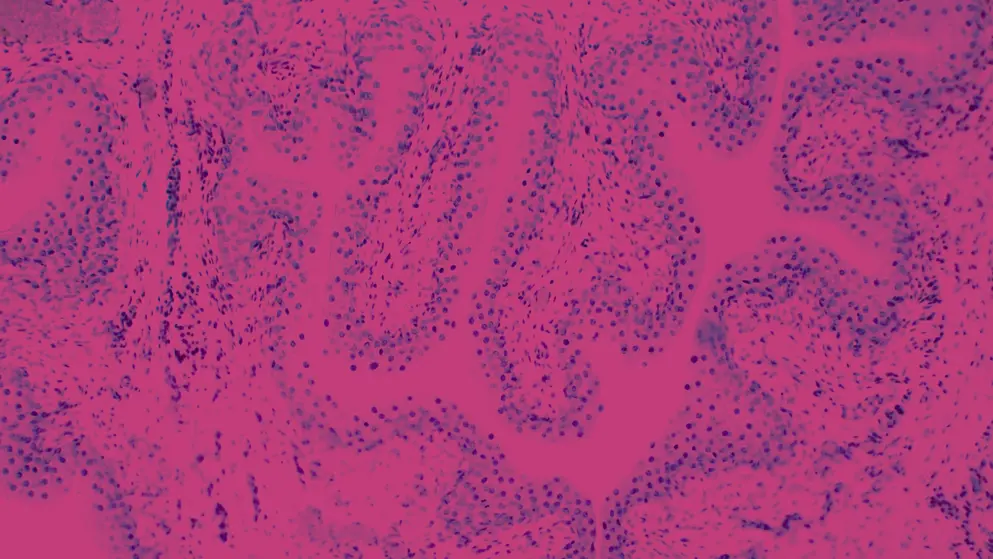
In recent years and especially months, because it's truly is an accelerated timeline, we've seen an explosion of AI and AI-driven tools trying to help the field of medicine and especially oncology, because there's a lot of data that has to be assimilated and a lot of data that has to be analyzed. And it's clearly benefits us, as clinicians, to lean on machine learning and AI algorithms. I was fortunate enough to be part of the team that presented this data at the EAU. And as you can see from the presentation, clearly using AI adds incremental benefit when it comes to risk stratification, putting patients in the appropriate buckets of treatment decision-making. It's not the only tool. So far this seems to be the best tool that at least I've been fortunate to have been part of. But there are other tools that use AI machine learning, and it's not just based on clinical parameters such as this one, but some of them actually look at tissue-based parameters, look at immunohistochemistry, look at other markers that are available. I think one of the things that we have to be optimistic about is where this will take us, but we also need to be a little cautious. Because sometimes what happens is when you have such fine level of detail that AI can help us identify, there's also a lot of noise that's come with it.
And we don't want to risk being paralyzed by having so much information at our hands that we lose the science and the art of actually taking care of human beings. And I fear that if this gets incorporated into EHRs or treatment algorithms without the appropriate clinical judgment, we might end up becoming algorithm-based clinicians, which clearly is not something that would benefit patients because the human element is still very important. And AI tool will never be able to replace me asking a patient, "Hey, what's important for you? Are you looking for a quality of life? Are you looking for a number of years?" That conversation still needs to happen at a human level. The use of quinolones in conjunction with BCG has been studied for many years over decades, and it was great to see those meta-analyses at the meetings, sort of looking at all the published data.
It makes mechanistic sense because you're decreasing the number of active bacteria. But I think one of the things that is very important for clinicians that read this meta-analyses or listen to the presentation or abstract and then try to implement this in a clinical practice is the timing is critical because the quinolones will kill BCG bacteria. We know this because we use this in patients that have BCG-osis or in patients that actually have tuberculosis, it's an active antibiotic. And if it's given too soon, in other words, if the patient takes it prior to BCG or right after BCG installation, there's a risk that it actually will kill the BCG bacteria and decrease the cytokine response.
So most of the studies that have looked at this that impress me and what I do in my practice is will recommend patients take quinolone prophylactically, 6–8 hours after they have voided the BCG. And again, because quinolone antibiotics can carry side effects and there's black box warnings in the United States against their use routinely, I restrict the use of quinolones for patients who are actually having side effects. And if they're having side effects, then it clearly helps them. But if they're not, then you're avoiding the risk of the quinolone side effects. So I think quinolones certainly have a role to play. I think they can be used selectively rather than everybody. And if you use them, it's very important to keep the timing of the quinolone administration in mind. The BCG unresponsive space has seen a huge explosion in agents being studied and approved in the United States. And there's of course off-label use of drugs as well, which have, in many parts of the country, become defacto standard. This leaves our patients and clinicians with a little bit of a conundrum because no patient wants to lose their bladder.
And if you ask a patient, "Would you like to try something else?" He or she will almost always say, "Sure." But it's up to us as clinicians to make sure that we are not letting our patients miss the window of opportunity for cure and educating them that each line of therapy does bring with it certain risks that the tumor may metastasize and become incurable even while we're trying to control the bladder. And that's where the onus is really on us. We need to make sure that we appropriately counsel the patients, and even more importantly, or just as importantly, stage the patient correctly, because at each evaluation, the question is not: Can I just do one more line of therapy? But the question is, is this patient at this time best treated with another line of therapy, whichever therapy it might be? Or are we getting to that edge of that window where if I try something else, I will lose the opportunity to offer my patients the chance of cure.
In 2025, we have technology, we have better imaging, we have markers, we have a whole bunch of tools at our disposal. And I really think we need to lean on the tools that we have and the knowledge that we've gained over the years and help our patients make informed patient-centric decisions at each stage of this question: "Is my patient doing well with more lines of therapy?"
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

