Congress highlights: NMIBC
How can clinicians select the best option for patients with non-muscle-invasive bladder cancer (NMIBC) that does not respond to Bacillus Calmette–Guérin (BCG)? Here, we round up the discussions and key data from the 2025 American Society of Clinical Oncology (ASCO) Genitourinary (GU) Cancers Symposium.
We also highlight research in intermediate-risk NMIBC, and Neal Shore (Carolina Urologic Research Center, Myrtle Beach, South Carolina, USA) discusses what the latest findings may mean for the care of patients with NMIBC.
Neal Shore discusses “the art of medicine” required to ensure maximum benefit from BCG maintenance therapy for patients with NMIBC in the face of multiple challenges. View transcript.
BCG-unresponsive NMIBC: Where next?
A key session on NMIBC addressed the question of which treatment to select for patients with BCG-unresponsive disease, with an expert panel talking through the options for a real-world patient case.
Session Co-Chair Bogdana Schmidt (Huntsman Cancer Institute at the University of Utah, Salt Lake City, USA), summarized the challenge, saying: “When there’s a small menu, you pick what you have. When there’s a larger menu, you have to think back to what do patients want and what can we do to meet their needs.”
Given all the options now becoming available, the “impressive” early efficacy of some of these in BCG-naive patients with high-risk disease, and the potential for highly individualized treatment using biomarkers and targeted therapies, Schmidt believes that BCG monotherapy “is not the way of the future.”
The panel rounded up the efficacy, safety, and treatment burden considerations for pembrolizumab, alone and combined with radiation therapy; for the interleukin-15 superagonist nogapendekin alfa inbakicept; and for the nonreplicating adenoviral vector-based gene therapy nadofaragene firadenovec.
The last of these options was approved around 2 years ago, and this year’s ASCO GU saw the first presentation of real-world data for the treatment, by Jacob Moyer (Graduate School of Biomedical Sciences, Phoenix, Arizona, USA) and colleagues. This showed positive outcomes in line with the efficacy seen in the clinical trials.
The 24 patients in the study had carcinoma in situ (CIS) with or without papillary disease. They were an average age of 71 years, 63% had prior intravesical chemotherapy, 26% had prior pembrolizumab treatment, and the median time from diagnosis to nadofaragene firadenovec treatment was 33 months.
At 3 months, 79% patients had a complete response (CR), with 84% of these maintaining CR at a median follow-up of 7.3 months. The most common adverse event (AE) was grade 1–2 bladder spasms (61%); just four patients experienced a grade 3 AE – two with fatigue, one with fever, and one with dizziness.
Does the real-world performance of nadofaragene firadenovec live up to its clinical trial promise? Shore gives his view and explains the rationale for assessing it in patients with intermediate risk. View transcript.
Returning to the panel discussion, despite the positive safety data supporting the available non-surgical options for BCG-unresponsive disease, for the specific case in question, the experts remained in favor of radical cystectomy based on the patient’s age and high-risk features (T1 disease plus CIS after progressing on gemcitabine and docetaxel). They proposed chemoradiation therapy or enrollment in a clinical trial as a back-up if the patient refused cystectomy.
Emerging therapies: An “exciting time”
The treatment menu for BCG-unresponsive NMIBC seems set to expand further, with panelist Girish Kulkarni (Princess Margaret Cancer Centre, Toronto, Ontario, Canada) highlighting the “diverse” mechanisms of action of in-development treatments, and saying that now is “an exciting time for all of us.”
The panelists highlighted several options with previously reported promising early data, namely:
- An intravesical delivery system known as “the pretzel,” which releases 225 mg gemcitabine over 21 days – tested in the SunRISe-1 trial
- The non-viral intravesical gene therapy detalimogene voraplasmid, showing encouraging data in the LEGEND trial
- The intravesical, conditionally replicating virus cretostimogene grenadenorepvec, assessed as monotherapy in BOND-003 and in combination with pembrolizumab in CORE-001
Another potential treatment approach for BCG-unresponsive, high-grade NMIBC is the PD-L1 inhibitor durvalumab plus intravesical gemcitabine and docetaxel, which is being tested as part of the ADAPT-BLADDER trial. Noah Hahn (Johns Hopkins University Sidney Kimmel Comprehensive Cancer Center, Baltimore, Maryland, USA) presented the phase 1/2 findings, involving a total of 40 patients.
The study participants received up to six cycles of durvalumab 1,500 mg every 4 weeks plus weekly intravesical gemcitabine 1,000 mg and docetaxel 37.5 mg. Monthly gemcitabine/docetaxel maintenance was recommended for patients with a CR.
Just 5% of the cohort had grade 3 AEs – two cases of pneumonitis and one of dyspnea – and there were no grade 4 AEs. One death occurred, which was considered unrelated to study treatment.
Overall, 89.2% of 37 evaluable patients had a CR, comprising 90.0% of 20 participants with CIS and 88.2% of 17 with pure papillary disease. Of the 16 patients evaluable at 12 months, 68.8% maintained a CR and 31.3% had recurrence.
"This is taking a proactive, some might argue a slightly more aggressive, approach." Shore discusses how therapeutic combinations including immune checkpoint inhibitors (ICIs) and chemotherapy might benefit patients, especially those with high-risk disease. View transcript.
UGN-102 for intermediate-risk NMIBC
Elsewhere at the conference, two posters presented by Sandip Prasad (Morristown Medical Center, New Jersey, Florida, USA) and team provided additional data from the phase 3 ENVISION and ATLAS trials. These tested UGN-102, a reverse thermal hydrogel containing mitomycin, administered as a monotherapy in ENVISION and in combination with transurethral resection of bladder tumor (TURBT) in patients with recurrent low-grade intermediate-risk NMIBC in ATLAS.
How might intravesical drug delivery systems influence clinical decision-making, and could they even affect decisions around TURBT? Shore offers his view. View transcript.
The latest findings show that the probability of maintaining a CR at 12 months was 82.3% in ENVISION and 79.7% in ATLAS. The probability with TURBT alone (in ATLAS) was 67.7%, equating to a significant 54% reduction in recurrence risk for ATLAS participants who also received UGN-102.
The most common AE was dysuria, occurring in about 20–30% of participants.
The researchers also reported that neither focality nor tumor burden significantly impacted the likelihood of CR at 3 months. As assessed in a subanalysis of ENVISION, CR rates were 79.3% and 82.9% in patients with multiple and single tumors, respectively, and were 82.8% and 73.2% in those with tumor burden of no more than 3 cm or greater than 3 cm, respectively.
How are the ways we address non-muscle-invasive bladder cancer (NMIBC) changing? Focusing on discussions held at the 40th Annual European Association of Urology (EAU) Congress, we provide a look at what’s next for NMIBC prognosis and treatment.
Artificial intelligence for NMIBC prognosis
Girish Kulkarni (University Health Network, Toronto, Ontario, Canada) presented PROGRxN-BCa, an artificial intelligence (AI)-based model intended to improve substratification of immediate-risk disease and predict progression risk in NMIBC.
The researchers used data from an NMIBC international cohort, training PROGRxN-BCa on data from 3,324 patients from four Canadian hospitals and then externally validating it using data from 9,335 patients across 30 North American and European institutions.
Of the total 12,659 patients, 1,405 (11%) developed progression over a median follow-up of 3.3 years.
Kulkarni reported that PROGRxN-BCa significantly outperformed the EAU NMIBC risk calculator, both overall and across multiple subgroups; the concordance indexes were 0.83 versus 0.76 (P<0.001) for training and 0.79 versus 0.71 (P<0.001) for external validation.
Looking specifically at 3,137 intermediate-risk patients, PROGRxN-BCa improved risk substratification relative to that based on the number of risk factors as per International Bladder Cancer Group (IBCG) recommendations. The AI approach generated risk tertiles with 5-year progression risks of 2%, 7%, and 17%, providing clearer separation between the first and second tertiles than the IBCG recommendations, which generated corresponding 5-year risks of 7%, 6%, and 20%.
Disitamab vedotin with BCG for HER2-expressing NMIBC
Yi Jun Shen (Fudan University Shanghai Cancer Center, China) presented phase 1 data for the novel antibody conjugate disitamab vedotin (DV) in combination with Bacillus Calmette–Guérin (BCG) for the treatment of high-risk NMIBC with HER2 expression. He noted this is the first study to evaluate DV in combination with BCG for this indication.
This may potentially provide a new bladder-sparing therapy for very high-risk NMIBC.
The trial involved two cohorts of patients with high-risk NMIBC with HER2 expression who had refused or did not meet the requirements for radical cystectomy (RC), divided into 15 who were unable to undergo complete tumor resection or had carcinoma in situ (cohort A) and five who underwent complete tumor resection (cohort B). All received eight cycles of intravenous (IV) DV (2 mg/kg every 3 weeks) and a minimum of 1 year of intravesical BCG.
Thirteen patients experienced treatment-related adverse events (TRAEs), with the most common being alopecia (45%), elevated alanine aminotransferase / aspartate aminotransferase (40%), sensory neuropathy (35%), and anorexia (10%). Two patients experienced grade 3 TRAEs: one instance of peripheral sensory neuropathy attributed to DV and one of hematuria attributed to BCG.
As of the cutoff date, the clinical complete response rate, which was the primary endpoint in cohort A, was 100% in 11 patients evaluated at 3 months and was also 100% in five evaluated at 6 months. In cohort B, the primary endpoint of event-free survival rate was 100% in three patients evaluated at 6 months.
Noting the promising efficacy and manageable safety profile of DV plus BCG, Shen highlighted the potential of this combination as a bladder-sparing therapy for people with very high-risk NMIBC with HER2 expression unable to undergo RC.
Prophylactic quinolones and BCG completion
BCG reduces recurrence and progression in high-risk NMIBC, but BCG-related adverse events are common and can often result in unwanted cessation of treatment (50–70% due to side effects). Chris Ho Ming Wong (The Chinese University of Hong Kong) suggested a solution to this recurring and significant issue: prophylactic use of quinolones.
His team’s systematic review and meta-analysis of the topic included five studies: four randomized controlled clinical trials and one retrospective study. This encompassed 445 patients: 194 who received quinolone and BCG and 251 who received BCG only.
Quinolone use was associated with a significantly lower likelihood of grade 2 or above toxicities (40.8 vs 54.7%; RR=0.79) and grade 3 or above toxicities (25.3% vs 36.4%; RR=0.70).
It was also associated with a higher BCG completion rate (83.0% vs 70.6%; RR=1.16), and Wong stressed that it did not compromise efficacy; there was no impact on 12-month recurrence rate or the rate of progression.
Wong emphasized the need for further study in this area, including the role of quinoline in maintenance BCG therapy and assessing whether the impact in induction therapy holds up in studies using more modern strains of BCG than were included in this meta-analysis.
Bel-sar: A virus-like-drug-conjugate for NMIBC
With a focus on addressing high recurrence rates in NMIBC, Seth Lerner (Baylor College of Medicine, Houston, Texas, USA) presented the results of a phase 1 trial looking at the safety and efficacy of belzupacap sarotalocan (bel-sar; AU-011) in patients with NMIBC.
Bel-sar is a first-in-class virus-like drug conjugate (VDC) derived from human papillomavirus (HPV). It is focally administered and has an immune ablative dual mechanism of action, selectively binding to tumor-expressed sulfate proteoglycans and inducing immediate tumor necrosis after near-infrared light activation and stimulating anti-tumor immunity. It has already demonstrated promising phase 2 results in melanoma.
This trial involved 15 patients with NMIBC who, 7–12 days prior to planned transurethral resection of bladder tumor (TURBT), received 100 µg bel-sar without near-infrared (690 nm) light activation (n=5) or bel-sar at either 100 µg or 200 µg plus light activation (n=10).
During 56 days of follow-up, no patient experienced any drug-related grade 2+ AEs, serious AEs, or dose-limiting toxicities.
All patients who received light activation had an immune response (immunocyte infiltration) in the target tumor and non-target tumor where applicable.
Furthermore, four of the five patients defined as at intermediate risk had a complete clinical response (cCR) of the target tumor, with three also having cCR of a non-target tumor. Among five high-risk patients, there was only one cCR of the target tumor, plus one cCR of a non-target tumor. However, three tumors were visibly smaller after treatment.
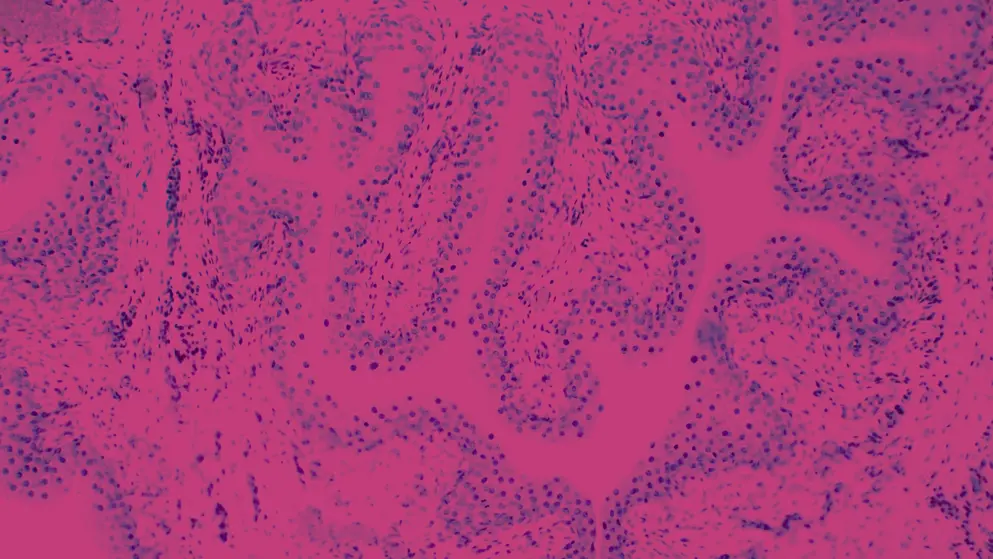
All treated and non-treated tumors in recipients of light activation showed marked CD4+/CD8+ T-cell infiltration. Lymphoid follicles were identified in five of seven target tumors.
Lerner concluded that a single, focal dose of bel-sar with light activation rapidly induces tumor necrosis, activates robust local immunity, and produces a broad urothelial field effect.
He said: “Next steps are to increase the dose up to 800, and then include more Ta high grade and carcinoma in situ.”
Join Ashish Kamat (University of Texas MD Anderson Cancer Center, Austin, USA) for his perspective on the latest updates in non-muscle-invasive bladder cancer (NMIBC) presented at the 40th Annual European Association of Urology (EAU) Congress (EAU25), ranging from artificial intelligence to novel treatment options. View transcript.
Chapters
00:01 Phase 1 findings for bel-sar in NMIBC
01:05 Updated phase 3 data for cretostimogene grenadenorepvec
01:54 Disitamab vedotin and BCG combination therapy
03:49 PROGRxN-BCa: AI for NMIBC
05:51 Prophylactic quinolones with BCG
07:32 Problems and controversies in NMIBC
AUA 2025 NMIBC round-up
Which “practice-changing, paradigm-shifting trials” in non-muscle invasive bladder cancer (NMIBC) released data at the 2025 American Urological Association (AUA) Annual Meeting?
Read on for the latest developments for patients with Bacillus Calmette–Guérin (BCG)-naive and BCG-unresponsive disease, and to hear why a prospective, observational study of radical cystectomy versus bladder-sparing treatment confounded the researchers’ expectations – check back here soon to hear clinician and patient advocate views on those results.
CREST findings support PD-1 blockade in BCG-naive patients
CREST is one of three ongoing trials assessing whether the addition of a PL-1 inhibitor can boost response in BCG-naive NMIBC, and is the first to report its findings.
Adding sasanlimab to first-time BCG induction and maintenance therapy resulted in significantly improved EFS in the CREST trial
Over a median follow-up of 36.3 months, the event-free survival (EFS) rate was 82.1% among the 352 patients who were randomly assigned to 4-weekly cycles of sasanlimab (maximum 25 cycles) in addition to BCG induction and maintenance.
By comparison, EFS in the 351 patients who received BCG only was 74.8%, amounting to a significant 32% relative difference in favor of sasanlimab. Presenter Neal Shore (Carolina Urologic Research Center, Myrtle Beach, South Carolina, USA) highlighted that the addition of sasanlimab halved the risk for recurrence of high-grade disease, at a rate of 7.4% versus 15.1% in the BCG-only group.
There was some variation in response between subgroups; Shore pointed out the stronger response to the addition of sasanlimab in people with carcinoma in situ (CIS) than those without.
Indeed, he highlighted the “rather compelling finding” that after 36 months the probability of a continued complete response in patients with CIS in the sasanlimab group was 91.7%, compared with 67.7% in the BCG-only group.
All trial participants had T1 disease that was high-grade Ta and/or CIS, and were stratified by the presence or absence of CIS.
The safety profiles were as anticipated for the drug classes. Grade 3 or 4 adverse events (AEs) occurred in 29.1% of the sasanlimab group and 6.3% of the BCG group, with the most common AE associated with sasanlimab being increased lipase levels.
Shore also noted that the rates of BCG maintenance discontinuation were similar in both treatment groups. “What that tells me is that adding sasanlimab did not impact the ability to deliver induction and maintenance BCG,” he said.
BOND-003 update confirms durable response in BCG-unresponsive CIS
Moving on to novel approaches for BCG-unresponsive NMIBC, Mark Tyson (Mayo Clinic, Phoenix, Arizona, USA) presented updated results from BOND-003, specifically the cohort comprising patients with CIS, with or without papillary tumors.
The 112 patients in this cohort received six weekly inductions with the intravesical, conditionally replicating virus cretostimogene grenadenorepvec (with a repeat course available for initial non-responders), followed by maintenance every 3 months in the first year and every 6 months in years 2 and 3.
At the March 2025 data cutoff, 75.5% of the cohort had a centrally confirmed complete response, with the 12- and 24-month rates being 46.4% and 33.7%, respectively, in 110 and 101 evaluable patients. The benefit was consistent across subgroups, regardless of factors including age, race, prior non-BCG therapies, and disease status at baseline.
Tyson stressed that “perhaps even more meaningful to patients” was the finding that, at month 24, 97.3% remained progression-free and 84.5% avoided radical cystectomy, “highlighting cretostimogene’s bladder-sparing potential.”
He noted that the longest duration of response to date is “45 months and counting,” and said the fact that many patients maintained complete response well after completion of treatment “supports the role of immune memory in mediating this long-term disease-free survival.”
Cretostimogene grenadenorepvec was “exceptionally well tolerated,” with all AEs being grade 1–2 and transient; the most common were bladder spasm (25.0%), pollakiuria (21.4%), and urgency (20.5%).
SunRISe-1: TAR-200 monotherapy promising regardless of disease stage
Another hopeful development for BCG-unresponsive NMIBC is advanced delivery systems for intravesical chemotherapy.
TAR-200 has delivered the highest single-agent complete response rate reported to date in BCG-unresponsive CIS
The phase 2 SunRISe-1 trial is testing the novel TAR-200 system, designed to provide sustained release of gemcitabine in the bladder. AUA attendees heard positive updates on outcomes for patients with and without CIS who received TAR-200 as monotherapy, delivered every 3 weeks for the first 24 weeks and every 12 weeks to week 96.
Joseph Jacob (Upstate Medical University, Syracuse, New York, USA) reported 1-year durability data for the 85 patients with high-risk CIS, with or without papillary tumors. He noted that only 3.5% of the patients were ineligible for radical cystectomy, with the vast majority having refused the procedure, saying: “This shows you how motivated patients were for bladder-preservation therapy.”
The complete response rate was 82.4%, which Jacob said is the highest single-agent complete-response rate so far reported. The median time to complete response was 2.8 months, the observed response rate at 12 months was 45.9%, and the estimated 12- and 24-month rates were 52.4% and 44.7%, respectively.
Just over half of the responses lasted for more than a year, and Jacob pointed out that most progression events occurred within the first year, after which “the curve flattens, which is a good predictor of durability.”
Felix Guerrero-Ramos (Hospital Universitario 12 de Octubre, Madrid, Spain) presented the findings for the 52 patients without CIS, reporting that disease-free survival in this cohort was 85.3% at 6 months and 81.1% at 9 months. The corresponding rates were 85.7% and 82.1% in the 59.6% of the cohort with high-grade Ta disease and 84.7% and 79.4% in the 40.4% who had T1 disease.
“This shows that, regardless of the T stage, TAR-200 is highly active in this population,” said Guerrero-Ramos.
The most common AEs across both cohorts were grade 1–2 pollakiuria and urgency, and approximately 13% of patients had a grade 3 or higher AE; these comprised urinary tract pain, bladder pain, urinary tract infection, pelvic pain, and urinary incontinence.
CISTO confounds expectations for QoL after radical cystectomy
The prospective, observational CISTO study was launched following a Bladder Cancer Advocacy Network patient survey that showed a high need for better information about radical cystectomy, including its optimal timing and how to balance it with bladder-sparing approaches.
Contrary to the researchers’ hypothesis, physical QoL was at least as good after radical cystectomy as after bladder-sparing interventions
John Gore (University of Washington, Seattle, USA) explained that the working hypothesis was that the 199 patients who underwent radical cystectomy would have poorer quality of life (QoL) 12 months later than the 371 who opted for bladder-sparing interventions.
The reality, however, was that the two groups had similar physical functioning on the EORTC QLQ-C30, which was the researchers’ primary outcome. This was true also for patients aged 75 years or older.
Moreover, the radical cystectomy group had significantly better global health on the EQ-5D than the bladder-sparing therapy group, and significantly better scores for emotional functioning, depression, and anxiety. They also had more positive financial outcomes.
Being a nonrandomized study, there were significant baseline differences between the groups. Patients who opted for bladder-sparing treatments were older than those who underwent radical cystectomy, were more often single and living in an urban location, and were less likely to have T1 disease or CIS. The researchers used targeted maximum likelihood estimation in their analyses to combat these differences.
The radical cystectomy group had initially poorer urinary health, but this improved over the study period until it was on a par with that of the bladder-sparing therapy group. However, sexual and bowel health remained worse.
Recurrence-free survival was better after radical cystectomy than bladder-sparing therapy, at 96% versus 67%. Other 12-month survival outcomes were similar between the groups.
Gore concluded that radical cystectomy “has, and should continue to have, an important role in the management of recurrent, high-grade non-muscle-invasive bladder cancer.”
“I think it’s immediately going to make a big splash.” Mark Tyson II (Mayo Clinic, Phoenix, Arizona, USA) discusses the latest from BOND-003 on the novel treatment cretostimogene grenadenorepvec. View transcript.
Chapters
00:05 About cretostimogene grenadenorepvec
01:18 BOND-003: Response and tolerability
03:12 What's next for BOND-003?
04:34 Into the clinic: Implications for practice
"I’m excited about non-muscle-invasive bladder cancer and immune checkpoint inhibition for lots of different reasons.” Thomas Powles (Barts Health NHS Trust, London, UK) discusses the CREST trial, including the rationale, previous findings, and phase 3 results presented at the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting. View transcript.
"It’s time to create new and novel agents.” Gary Steinberg (Rush University Medical Center, Chicago, USA) discusses cretostimogene grenadenorepvec, covering its mechanism of action and the associated clinical trial results. View transcript.
Which emerging therapies for non-muscle-invasive bladder cancer (NMIBC) could shift the treatment landscape?
Read our highlights from the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting, covering key developments, including PD-1 checkpoint inhibition with Bacillus Calmette–Guérin (BCG), HER2− and TROP2-targeted antibody–drug conjugates (ADCs), oncolytic viral therapy, and urinary tumor DNA (utDNA) to support resection decisions.
To hear the experts’ views of this growing toolbox, watch our interviews with the presenters of key trial data under ASCO 2025: Expert reflections.
PD-1 blockade in BCG-naive high-risk NMIBC: CREST update
The CREST investigators previously reported that 3-year event-free survival (EFS) rates were higher with sasanlimab in combination with BCG than with BCG alone in BCG-naive patients with high-risk NMIBC.
The new data presented at ASCO 2025 show that this was the case for those with higher-risk disease at baseline. Among patients with carcinoma in situ (CIS), 3-year EFS reached 83.0% with the combination versus 71.8% with BCG alone. For those with T1 disease, rates were 81.3% and 72.2%, respectively.
Sasanlimab plus BCG improved 3-year EFS in CIS and T1 subgroups compared with BCG alone
Thomas Powles (Queen Mary University of London, UK) presented these investigator-assessed, post hoc subgroup analyses, which were not powered for direct comparison but explored outcomes in relevant high-risk cohorts.
He reported that the consistent effect across the CIS and T1 subgroups occurred despite PD-L1 expression being notably lower in patients with CIS. There was also no difference within these subgroups when stratified by high versus low PD-L1 expression.
The safety profile of sasanlimab in combination with BCG was consistent with known immune checkpoint inhibitor-related events. Treatment-related grade ≥3 adverse events occurred in 29% of patients receiving the combination, with increased lipase levels and hematuria being the most common events. No treatment-related deaths occurred, and no new safety signals were observed.
A phase 3 study is planned to assess sasanlimab in combination with BCG in patients with BCG-naive CIS and papillary disease.
utDNA may help identify candidates likely to benefit from repeat TURBT
A retrospective analysis from the Second Hospital of Tianjin Medical University, in China, assessed the utility of utDNA to inform decisions on repeat transurethral resection of bladder tumor (re-TURBT) in patients with high-grade Ta or T1 NMIBC.
utDNA showed a positive predictive value of 89.7% for residual tumor at re-TURBT
Among 130 patients included in the analysis, 39 had positive utDNA 1 week after initial TURBT. Of those, 35 (89.7%) had residual tumor confirmed by pathology at re-TURBT. utDNA demonstrated 76.1% sensitivity and 95.2% specificity in detecting residual disease.
A positive utDNA result was also independently associated with increased risk of recurrence, with a hazard ratio of 4.48 (P<0.001). Zihan Xue and co-researchers concluded that utDNA may serve as a non-invasive biomarker to support decisions around repeat resection in patients with residual disease and help avoid unnecessary procedures.
A randomized phase 2 study is planned to further evaluate the role of utDNA-guided re-TURBT in high-grade NMIBC. If validated, utDNA testing may contribute to more personalized treatment strategies in this setting.
In-progress trials shaping future of NMIBC treatment
Alongside the latest data, researchers also provided updates on recently launched and in-progress trials in NMIBC.
HER2-targeted triplet therapy for high-risk NMIBC
The novel triplet regimen being assessed in PUNCH03 combines checkpoint inhibition, targeted therapy, and BCG in patients with HER2-positive disease
The open-label phase 2 study is evaluating disitamab vedotin, tislelizumab, and BCG as a bladder-sparing regimen in patients with HER2-positive high-risk NMIBC. All patients are BCG-naive with high-grade Ta or T1 tumors and HER2 expression confirmed by immunohistochemistry.
Zongren Wang (Sun Yat-sen University, Guangzhou, China) and colleagues designed the protocol to include initial TURBT followed by one cycle of disitamab vedotin and tislelizumab. After a second TURBT, patients receive tislelizumab every 3 weeks, plus three to five cycles of disitamab vedotin followed by BCG induction and maintenance treatment.
The primary endpoint is 12-month recurrence-free survival, with a predefined target of ≥85%. Secondary endpoints include bladder preservation rate, overall survival, and safety.
The study is ongoing, and monitoring for treatment-related adverse events continues.
CORE-008 aims to expands intravesical options with oncolytic virus and gemcitabine
Cretostimogene grenadenorepvec is a replication-selective adenoviral vector that targets tumor cells with retinoblastoma pathway alterations and expresses granulocyte-macrophage colony-stimulating factor. It is administered intravesically with a permeability enhancer.
In the CORE-008 trial, Gary Steinberg (Rush University, Chicago, Illinois, USA) and colleagues are evaluating cretostimogene as monotherapy and in combination with gemcitabine in patients with high-risk NMIBC, including those who are BCG-naive, BCG-exposed, and, for those in the combination treatment cohort, BCG unresponsive. The combination is being tested using both sequential and concurrent dosing schedules.
The goal of the study is to assess safety, tolerability, and preliminary efficacy, including complete response in patients with CIS and high-grade EFS in those with papillary tumors.
For additional context on the cretostimogene clinical trial program, watch our interview with Steinberg.
TROP2-targeted ADC enters early testing in intermediate-risk NMIBC
Early-phase trial evaluates sacituzumab tirumotecan as localized therapy in NMIBC
Sacituzumab tirumotecan (sac-TMT), a TROP2-targeted ADC, is under investigation as a localized therapy for intermediate-risk NMIBC in the TroFuse-027 study. Joshua Meeks (Northwestern University, Chicago, Illinois, USA) presented early-phase data from this ongoing phase 1/2 open-label study, which includes patients with recurrent low-grade Ta tumors, negative urine cytology, and no evidence of high-grade disease. The trial excludes patients with prior BCG-unresponsive disease or concurrent CIS.
In part 1 (dose-escalation phase), patients receive sacituzumab tirumotecan once weekly for 6 weeks, to assess safety and determine the recommended phase 2 dose. Secondary objectives include pharmacokinetics and preliminary efficacy, measured by complete response at week 12.
At week 12, patients undergo cystoscopy, cytology, and biopsy. Those with persistent or recurrent tumors undergo TURBT, followed by continued observation per study protocol.
The investigational drug is a TROP2-directed ADC that delivers a belotecan-derived topoisomerase I inhibitor intended to act locally within the bladder to reduce systemic exposure.
The study is currently still enrolling patients, with part 2 planned to further evaluate safety and efficacy at the optimal dose established in part 1.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

