HRR Mutation Testing in mPC
Transcript: Stefanie Zschäbitz on TALAPRO-2
Stefanie Zschäbitz, PD, MD
Interview recorded June 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
So, the TALAPRO-2 Study was a phase 3 study that recruited patients with first-line mCRPC, and those patients were asymptomatic or mildly asymptomatic and they were one-to-one randomized towards TALA + ENZA versus ENZA + Placebo, and we recruited two cohorts, so it's basically two studies in one. The first cohort was Cohort 1, which recruited patients independent of the HRR status within their tumor, and the data that I recorded at ASCO was from Cohort 2, which is a cohort of patients whose tumors harbor HRR alterations within their tumors, and those HRR alterations were prospectively analyzed.
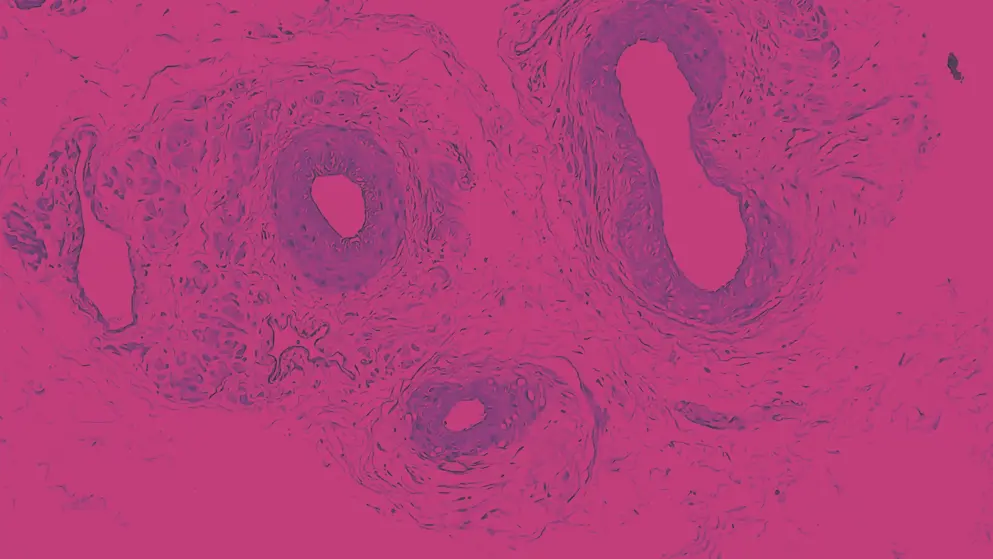
The primary endpoint of the study was rPFS and the key secondary endpoint of the study was OS, and both endpoints have been presented previously, they were both positive for both cohorts. And the data that we had at this ASCO was about subgroup analysis by gene, and we had declared 12 genes HRR deficient, and we concentrated on 6 of the 12 genes, because 92% of the population had at least one alteration in one of these six genes, which means the subgroups would've been really small if we would have added all 12 genes, so we concentrated on those six genes, and a finding that we had, we were looking at several endpoints of efficacy, rPFS, OS, PSA response, time to PSA progression over response rate, we were looking specifically at those by gene subgroups, And we saw that it is not only the BRCA1 or the BRCA2 that have a benefit from the combination treatment with TALA + ENZA, but also other subgroups such as CDK12, for example, or PALB2, and I think that is an important finding, because, we as clinicians, have to make decisions when patients have those alterations as well.
So the FDA approval and the EMA approval differ, for the EMA approval, the label is independent of HRR status, whereas in the FDA, the label is for HRR deficient tumors, so especially when we consider patients for treatment with TALA + ENZA, I think it's important to have the HRR status, even if it's not necessary within the European Union, but, you know, to know if a patient would have other options such as in a BRCA mutated patient, you could also go with Olaparib monotherapy, and having this whole picture, I think is really important to make a good decision for the patient, but again, as I said before, it's not only the BRCA1/BRCA2 patients that have a benefit from the treatment, obviously, if you go into subgroups, those analyses are not adequately powered to detect any statistically significant difference, the power calculation is met for primary, key secondary endpoint and those were positive also for OS, which is important because that is something that we don't see in a lot of trials nowadays, as we have so many subsequent treatment lines. But I think the main finding definitely is that it is not only BRCA1 and BRCA2 who have a benefit, although the benefit is smaller in patients with non-BRCA HRR alterations.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

