HRR Mutation Testing in mPC
Transcript: Gerhardt Attard on AMPLITUDE
Gerhardt Attard, MD, PhD, FRCP
Interview recorded June 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
The AMPLITUDE trial tested niraparib and abiraterone in metastatic castration-sensitive prostate cancer, harboring alterations in genes involved in homologous recombination repair So defects that resulted in loss of homologous recombination repair. The rationale for testing this combination in mCSPC is manyfold. PARP inhibitors have been approved for HRR-altered metastatic castration-resistant prostate cancer for several years. And there are two challenges that we aimed to address. The first is that resistance commonly develops when we use PARP inhibitors alone for mCRPC, the time to radiographic progression is a median of less than 12 months. And the second challenge is that we had evidence to support combining inhibition of both PARP and the androgen receptor pathway as cooperative if not synergistic, but we now use androgen receptor pathway inhibitors for mCSPC. So the population of patients who could receive a combination of a PARP inhibitor and an inhibitor of the androgen receptor pathway was ever shrinking and probably becoming less and less relevant.
So the top line efficacy and safety results on the Amplitude trial I presented at ASCO. Let's start with efficacy. The amplitude trial met its primary endpoint. This was a significant improvement in time to radiographic progression-free survival. The trial used a graphical approach to test three endpoints, rPFS and then two key secondary endpoints in predefined molecular subgroups for each endpoint. And that started with BRCA, so cancers that had a BRCA mutation. And lastly, finished off with the whole intention to treat population, which as you've gathered from the title, is cancers with an alteration in any homologous recombination repair gene. The hazard ratio in the BRCA mutant population is 0.52, so that's close to halving the risk of radiographic progression of death. And then the whole HRR population, it was 0.63. So very statistically significant benefit and clinically significant benefit for adding niraparib to abiraterone and ADT in the setting of mCSPC. The other two key secondary endpoints, the first one was time to symptomatic progression. So that was time to an objectively determined patient-centric event, which is a requirement for an intervention or radiation or a new cancer treatment. And the hazard ratio for that endpoint was 0.44. So a 56% reduction in risk in the BRCA mutant group and 0.5 or 50% reduction in risk of symptomatic progression in the whole HRR population.
The second key secondary endpoint is overall survival, which at the time of reporting at this interim analysis, we had half the number that the trial had recorded, half the number of target events that are required for the survival. So overall survival is immature, but we see a promising, a trend towards benefit from adding niraparib to abiraterone. And the hazard ratio, the BRCA population is 0.75 and the whole HRR 0.79 and about 36% patients treated with placebo received a PARP inhibitor after progression on the trial. So there's a fair amount of crossover and at this interim analysis, a hazard ratio estimate which is well below one, but not at this point statistically significant. So we cannot be certain that niraparib added for mCSPC improves overall survival. In terms of safety, we have experience with this combination, as I said at the start in mCRPC, so patients who have progressed on first line hormone therapy and the side effects we observed are in the same profiles. So the systems that are most involved are the hematological and cardiovascular systems. Anemia, the most common grade three or four side effects, I should say more side effects with niraparib. So 15% more grade three or four side effects with niraparib, which were reported in 75% of patients versus 59% in placebo. But those side effects were in systems we know are side effects of care with PARP inhibitors, anemia, the most common, 99 patients had grade three, two had grade four, so that's about 29% of patients treated with niraparib. Hypertension was also grade three four, hypertension was also more common with niraparib.
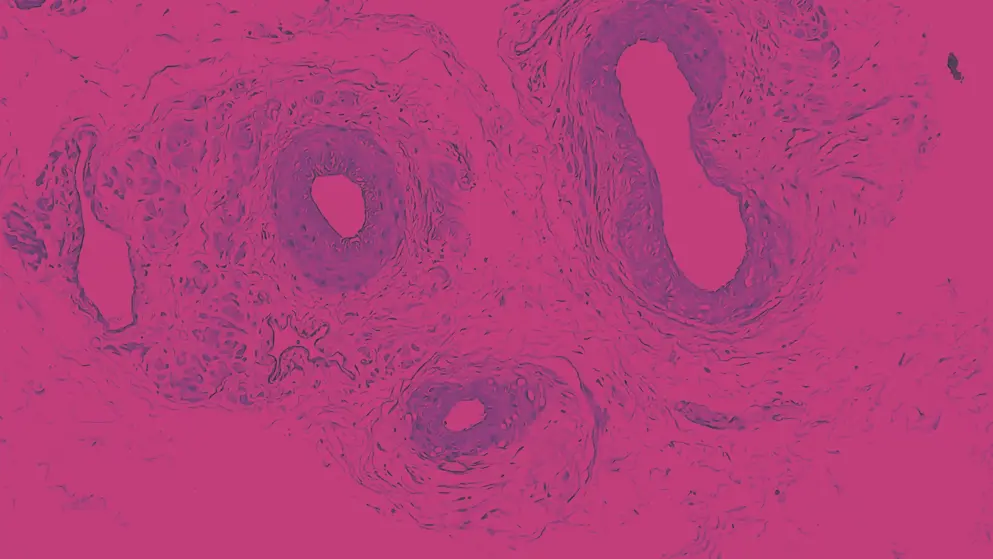
Then there's an uncommon side effect, in fact, one could say rare and that's myelodysplastic syndrome, but it's of interest 'cause long-term PARP inhibition increases the risk of MDS and other leukemias. There was one case treated with niraparib where MDS was diagnosed in the time of reporting and that patient had a CHEK2 germline mutation. We continue to follow up patients and over the next few years, we will report updated analysis for survival and also for longer term side effects. If the niraparib trial is implemented, this will have an effect on genomic testing, especially in Europe, where currently we test tumours for alterations in HRR genes once a patient has developed CRPC, this comes with a number of logistical challenges. The first is this could be several years after a patient is diagnosed, so the tumor sample is offsite in another place, has to be brought in, has to be reviewed by a pathologist or may not be found. And then when it is found, there's a relatively high failure rate for obtaining a sequencing result. This is about 10 to 40% depending on the age of the sample, the sequencing test, et cetera. By moving testing upfront to mCSPC, we're going to see a much higher success rate for the sequencing test. And logistically, this is going to be much more straightforward 'cause it could be ordered as a reflex test by the pathologist when the diagnosis of metastatic CSPC is made.
So, although there initially may be an increased burden on healthcare systems as they're testing mCRPC and mCSPC in the longer run, upfront testing will probably be logistically easier for our healthcare providers, identify more patients because of a higher success rate, and from the results I presented from the AMPLITUDE trial be associated with greater efficacy and greater benefit for patients.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

