HRR Mutation Testing in mPC
Transcript: EAU25: HRR in mCRPC – Expert takeaways
Pedro Barata, MD, MSc, FACP
Interview recorded April 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
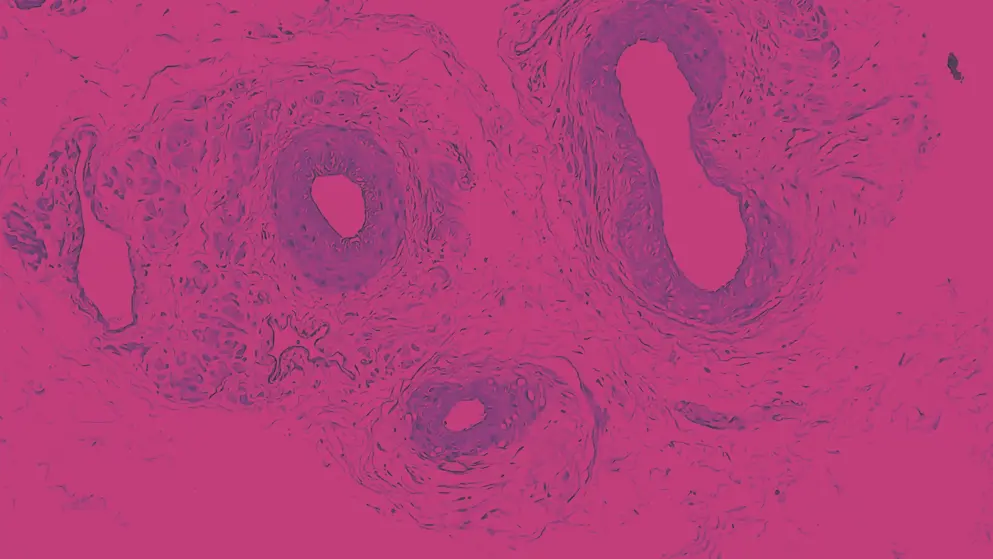
So the question of this abstract is a relevant one. This is actually a single-arm phase 2 study of a new PARP inhibitor, pamiparib, for patients with metastatic CRPC. This is work mainly done in China at Sun Yat-sen University Cancer Center, and you know, and we had 42 patients enrolled with mCRPC. Of those, about 11 or so, got BRCA1, BRCA2, and most had, you know, HRD score, which is basically homologous recombination deficiency score which was defined as high, over nine. And the majority of patients had a high score. So, just a background, we know PARP inhibitors work in monotherapy when we have a presence of homologous recombination deficiency, particularly BRCA alterations. They do also show activity beyond BRCA. We do have current approvals for mCRPC with olaparib and rucaparib as monotherapy. And then combination of PARP inhibitors where backbone ARPI have also shown significant activity, not only in homologous recombination deficient tumors, but also at least with a combination of enzalutamide with talazoparib beyond HRR.
So we're looking at signal of efficacy for HRR negative or undetermined. You know, so with that said, going back to this PARP inhibitor, basically, the authors report activity of these PARP with responses that are, you know, that are kind of expected. You know, we're looking at actually 33% responses in patients with BRCA mutations, overall, 17.6%, you know, I would argue this a single-arm, it's a proof of concept. We do see signal, I'm not sure it's the strongest signal we've seen for PARP inhibition. I'm not aware of significant studies with this particular PARP in prostate cancer, you know, at least in this side of the world, in US. I would say we do see a signal. We also look at PFS, or they, the authors, look at PFS 7 months, which to me actually sounds a little bit underwhelming. I do expect for patients with HRR, particularly BRCA, we do know that we can, you know, we can expect longer time to progression. And so I would say PARPs continue to work in prostate cancer. I'm not sure where we are with the different PARPs and different combinations. This will be the one, I think it kind of goes in line, perhaps the data here and there might be a little bit underwhelming, but nonetheless, it's important to reflect on the importance to identify these patients. It depends on the ability to test them, to do genetic testing. And I think an important message of showing work like this at the EAU is to remind doctors around the world that genetic testing identifies these patients for PARP inhibitors in monotherapy. With combinations is a different conversation, and so I think this study has the merit of reminding us of that. So, so that would be my take on this particular study.
So this fantastic work by Dr. Olmos, Dr. Castro and the team, the Spanish effort basically looking into outcomes for patients with homologous recombination repair gene. So we know HRR has prognostic value in addition to predictive value. Previously the authors have reported specifically on the prognostic value of BRCA1 and 2, but the prognostic value of the other non-BRCA HRR, it's for the most part not entirely known. And so it's data looking at how do patients do with non-HRR, with non-BRCA HRR disease do perform in terms of prognosis is of relevant value. So that's what Dr. Olmos and the team do in this work. They basically, you know, break down by genomic alterations of interest like ATM, CDK12. They show you the BRCA for comparison. They actually show you BRCA1 separate from BRCA2, and then you go through the other HRR and they show you data for progression-free survival and overall survival. And I think it's pretty obvious to me that what you can appreciate is the different contribution of the genomic alterations to the prognosis of these patients, right? So you can clearly see it's not just BRCA2 that determines a poor prognostic value or factor. Rather you have other genomic alterations, you know, look at BRCA1 and others that in fact patients don't do great unfortunately.
And so this really basically adds to the body of work showing that HRR has prognostic value and we need therapies that bring, that eliminate or minimize hopefully these negative prognostic value, bring them to similar to prognosis of patients who do not harbor, whose tumors do not harbor HRR. So this is data that I'm looking forward to see it published. It's relevant, comes out of these effort called PROCURE which is a platform for biomarkers. A Spanish group has done fantastic work here. And so I would recommend everybody to look into the details and I'm sure the paper will come out soon, looking at specifically prognostic value of non-BRCA HRR, alterations, and very elegantly presented. These work presented at EAU explores or do an ad hoc analysis on the BRCA status of patients enrolled in the ARTO study. Just a reminder, ARTO, look at patients with oligometastatic CRPC to be randomized to abiraterone, which is standard of care for metastatic CRPC, or abiraterone along with radiotherapy or stereotastic body radiotherapy, better said, as a metastasis directed therapy, right?
So basically we have Abi or Abi plus SRS and we do know that it show a good improvement in terms of biochemical response. In other words, PSA response, as well as progression free by adding SRS to the oligo sites of Mets, right? Which makes sense. What this study does, it takes one step further and looks at specifically the benefit of that approach of bringing radiation on top of abiraterone, based on BRCA status. And the thought process behind it, you know, is that we know that BRCA represents a poor prognostic value. And so the question is, if you expect patients to progress quickly, is it worth to explore local therapy with radiosurgery on top of an ARPI like abiraterone. So that's really in essence what's behind the concept presented here. Bottom line, the benefit of adding radiation to abiraterone was confirmed in the group of patients with BRCA negative, were tested. And you also see, you know, a signal in, you know, you do see BRCA positive patients has a low hazard ratio of 0.5. However, you know, small sample size gives you wide confidence interval. So you cannot conclusively say, and it would be a proof of concept, I guess, and a hypothesis generator at most, you cannot definitively say that bringing radiation for patients who are BRCA positive in the context of oligometastatic CRPC is the thing to do. However, I do think in clinical practice, if we have a BRCA positive patient in mCRPC, most of us if possible are gonna bring a PARP inhibitor perhaps on top of an ARPI, right?
So we are seeing less of patients getting to mCRPC without being exposed to an ARPI. So this study was designed getting the abiraterone as the ARPI for mCRPC. I think as things go, move on, I think we'll be seeing patients who might have gotten an ARPI normal sensitive disease for which these would probably would not be data to support doing such an approach later on. But local therapy has been over and over again shown an intelligent approach for patients with metastatic disease, particularly, for patients with limited amount of disease. So this is interesting data. I think you, you know, the group of patients with, who have BRCA positive is limited, the final results. To me, that'll be the most interesting piece, right, because these patients have a poor prognostic value. We know they progress very quickly on ARPI and I think currently and moving forward, the questions asked here is merging into something else as more patients get an ARPI before getting to mCRPC and also with a combination of ARPI and PARPs being available, right, that's the new question, right? Because we have a studies like BRCAAway looking at Abi or olaparib and crossover or combo that you can see in that proof of concept, that doing combo upfront is superior to actually do one followed by the other.
So I think as we move along, I do anticipate more studies looking into the value of local therapy in the contemporaneous approach. Nonetheless, it is an important effort. ARTO study is an interesting study. And so kudos to the authors for conducting such an analysis. It's a very, or particularly relevant question in metastatic prostate cancer. Why? Because often tissue is either not available, it's very old and there are logistical and methodological challenges with biopsying bone, for example, that leads to many patients not getting available tissue, archival tissue, or not able to get a biopsy to go after molecular profiling of those tumors. So the question is always, can we go with circulating DNA testing or liquid biopsy as a surrogate for what's going on at the tissue level, being tissue testing considered still gold standard? And the answer in short is yes. We have many datasets showing that there is high levels of concordance, 80%, so perhaps higher of, you know, liquid biopsies compared to tissue testing. And so these two studies look at, one, look at the role of circulating tumor DNA for patients with CRPC who fail Abi or Enza. There's many other studies out there looking into something very similar. The bottom line is you do find genomic alterations that you expect to find, including up to a third of HRR among other alterations of interest. You do see, you know, the number of treatments with or without detectability of ctDNA and how that impacts prognosis.
This data already exists. There's more datasets kind of are going in the same direction. To me, I find the Italian study more interesting in the sense that it's looking specifically of the BRCA alterations detected by liquid biopsy. So you basically look at things like gene deletion or point mutations or gene loss or exon rearrangements, and you kinda look at the breakdowns. It's a very interesting study. By the way, they do detect alterations in the BRCA gene in about 20% of the times, which is, you know, and this is a heavily treated population. And so that's, to me, that's of interest, right? Because we need to understand what genomic alterations represent what in terms of predictive value in addition to, as we know, giving a prognostic and pro-prognostic value to these patients. So I think this Italian effort, it's an interesting one. It confirms again that genomic alterations are common. We should test these tumors. We can understand a little bit more the specifics around what type of genomic alterations we identify in prostate cancer, and the same is true for the Asian study in regards to what's going on at the tumor level in circulating tumor DNA, who progressed on prior ARPI of Abi and Enza. So important data aligned with other things. I think I, perhaps, looking at the specific genomic alterations of BRCA is of interest because the efforts moving forward are trying to understand can we go beyond a genomic alteration? What does that mean, right? They probably mean different things. So this study goes in that direction, and so, you know, it's good effort from the authors. PROact study is a very interesting study, very timely, I would say, good effort from the group in China.
Basically, looking at the combination of abiraterone with olaparib for metastatic hormone sensitive disease, and looking specifically at patients with HRR positive disease. So it's very, very interesting. It's a proof of concept, it's a phase 2 study, single-arm study, so everyone got the combination. And why is it timely? Well, because we are about to find out results or the important trials in this space with PARP inhibitors are about to read out amplitude with niraparib and abiraterone. We're gonna see TALAPRO-3 ring out soon as well with enzalutamide, talazoparib. And we did see data with this combination versus sequencing in the CRPC setting, also an investigative initiated study in that setting. And so it's really welcome, you know, to look at this data. By the way, this was a quarter of 30 patients, you know, and we're talking basically everybody with newly diagnosed metastatic hormone sensitive disease and everybody got the combination of abiraterone with olaparib. It's quite interesting to see that PSA responses were achieved in all patients, the 30 patients. Almost everyone got a PSA 90. So that means 90% decline in PSA compared to baseline. And the follow-up for this study was over years, like 14 months and nobody has progressed with PSA and I would assume, you know, not in scans either at the time of the data analysis. So that means is I would love to see this follow-up being 3 years, because you know, we can immediately understand whether or not these patients seem to be doing better than what we expect. Just a reminder, patients with newly diagnosed metastatic disease, 70% high volume in this study, these patients tend to progress in less than 3 years, usually in 2 years or less. So volume of the disease, timing of metastatic disease predicts prognosis and patients who do the worse are those with, tend to be the ones with high volume newly diagnosed disease.
So it will be very interesting with longer follow-up to see how these patients do. But this is a biomarker based study, it is a proof of concept. It makes all the sense to bring a PARP inhibitor in this setting. I'm not really surprised to see, but this is one of the first times I do see data in this space, in this fashion. So I would argue this is very important proof of concept that might be confirmed in larger efforts that are currently ongoing in a readout soon. So kudos to the authors. Very important study, I think. I predict the paper will be published in a high impact factor because it shows us where we are all interested in seeing should we move PARP inhibitors sooner in the spectrum of the metastatic disease. And these data seems to say likely yes, although it's premature, specifically, because of the short follow-up. But this is very promising results, and you know, it will, I'm looking forward to see the definitive phase 3 data reading out. But very good effort from these authors. Really, congratulations to them, it's really a good question that they're trying to answer here.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

