Publication digests
APPEAR-C3G trial
Read our publication digest to learn about the design of the APPEAR-C3G trial, which is investigating the efficacy and safety of an alternative complement pathway inhibitor, iptacopan, in patients with C3 glomerulopathy. Based on details reported in Bomback et al. (20221):
- Learn about the trial rationale and aims
- Explore aspects of the trial design in detail
- Consider the benefits and limitations of the trial design
Alternative complement pathway inhibition with iptacopan for the treatment of C3 glomerulopathy - study design of the APPEAR-C3G trial
Source publication: Bomback AS, Kavanagh D, Vivarelli M, Meier M, Wang Y, Webb NJA, Trapani AJ, Smith RJH. Kidney Int Rep. 2022; 7:2150–21591.
C3 glomerulopathy (C3G) is a chronic and rare kidney disease2,3 most often diagnosed during childhood and young adulthood4. C3G has a poor prognosis, with around 30–50% of people with C3G reaching end-stage kidney disease (ESKD) within 10 years of diagnosis5.
C3G is caused by dysregulation of the complement system, driven by excessive activation of the alternative complement pathway4. It is histologically characterised by dominant deposition of the complement component C3 in the glomerulus3.
Current treatments for C3G are limited to supportive measures to minimise proteinuria and suppress kidney inflammation5, and there is a need for approved treatments that target the underlying pathophysiology of the disease4,6
Rationale for the APPEAR-C3G trial
Considering the key role of complement dysregulation in the pathophysiology of C3G, investigational treatments that inhibit the complement system are in various stages of clinical development1,4,7,8.
Iptacopan is an oral, first-in-class, potent and selective inhibitor of Factor B, a key component in the alternative complement pathway1. In an open-label, non-randomised Phase 2 study, iptacopan treatment was associated with a reduction in proteinuria and C3 deposit scores in C3G patients with native and transplanted kidneys, respectively9,10.
APPEAR-C3G is a randomised, double-blind, placebo-controlled Phase 3 trial with an open-label period, that has been initiated to investigate the efficacy and safety of iptacopan in people with C3G1
APPEAR-C3G trial population
The APPEAR-C3G trial is enrolling adults who meet the following inclusion criteria1:
- Age ≥18–≤60 years
- Biopsy-confirmed C3G in the 12 months prior
- Reduced C3 (<77 mg/dL), proteinuria ≥1.0 g/g, and estimated glomerular filtration rate (eGFR) ≥30/mL/min/1.73 m2
- Taking maximally recommended or tolerated dose of angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor blocker (ARB) for ≥90 days
Exclusion criteria include organ transplant, use of complement inhibitors or immunosuppressants within 90 days of study drug administration, rapidly progressive crescentic glomerulonephritis on renal biopsy with interstitial fibrosis/tubular atrophy, or monoclonal gammopathy of undetermined significance1. More detailed trial inclusion and exclusion criteria are available online1,11.
A total of 68 participants are planned for enrolment in the study1. This is based on a sample size calculation to ensure sufficient power to test superiority of iptacopan versus placebo on proteinuria reduction (i.e. at least 80% power at the 1-sided 0.025 significance level)1.
APPEAR-C3G trial design
The overall design of the APPEAR-C3G trial is illustrated in Figure 1.
Figure 1. Design of APPEAR-C3G trial (Adapted1). The first 6 months of the study is randomised, double-blind and placebo-controlled, and the second 6 months is an open-label treatment period. After the end of the study, participants will have the option to roll over into an open-label extension program1. ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blocker; BID, twice daily; C3G, C3 glomerulopathy; n, number of participants; r, randomisation.
APPEAR-C3G trial outcomes
The objectives and endpoints used for the double-blind and open-label treatment periods of the APPEAR-C3G trial are summarised in Table 1 and 2, respectively.
Table 1. Objectives for the double-blind treatment period of APPEAR-C3G1. AEs, adverse events; AESIs, adverse events of special interest; ECG, electrocardiogram; eGFR, estimated glomerular filtration rate; FACIT-Fatigue, functional assessment of chronic illness therapy-fatigue; hr, hour; UPCR, urine protein:creatinine ratio. *The investigators noted initiation or intensification of antiproteinuric therapies or renal replacement therapy will be considered as treatment failures and therefore become part of a composite endpoint definition1.
| Objectives | Endpoints |
| Primary | |
| To demonstrate the superiority of iptacopan vs placebo on proteinuria (UPCR) reduction at 6 months | Log-transformed ratio to baseline in UPCR (from a 24 hr urine collection) at 6 months |
| Secondary | |
| To demonstrate the superiority of iptacopan vs placebo on improvement from baseline in eGFR at 6 months | Change from baseline in eGFR at 6 months |
| To demonstrate the superiority of iptacopan vs placebo in the proportion of patients who achieve a composite renal endpoint at 6 months | The composite renal endpoint is met if the following criteria are satisfied at the 6 month time point*: (i) a stable or improved eGFR compared to the baseline visit (≤15% reduction in eGFR), and (ii) a ≥50% reduction in UPCR compared to the baseline visit |
| To assess the effect of iptacopan vs placebo on reduction of glomerular inflammation in the kidney at 6 months | Change from baseline in disease total activity score in a renal biopsy at 6 months |
| To assess the effect of iptacopan vs placebo on patient-reported fatigue at 6 months | Change from baseline to 6 months in FACIT-Fatigue score |
| To evaluate the safety and tolerability of iptacopan vs placebo during the 6-month double-blind period | Vital signs, ECGs, safety laboratory measurements, AEs, AESIs |
Table 2. Objectives for the open-label treatment period of APPEAR-C3G1. AEs, adverse events; AESIs, adverse events of special interest; ECG, electrocardiogram; eGFR, estimated glomerular filtration rate; FACIT-Fatigue, functional assessment of chronic illness therapy-fatigue; UPCR, urine protein:creatinine ratio. *The investigators noted initiation or intensification of antiproteinuric therapies or renal replacement therapy will be considered as treatment failures and therefore become part of a composite endpoint definition1.
| Objectives | Endpoints |
| Primary | |
| To evaluate the effect of iptacopan on proteinuria (UPCR) at 12 months | Change from baseline in log-transformed UPCR at the 12 month visit (both study treatment arms) Change in log-transformed UPCR from the 6 month visit to the 12 month visit in the placebo arm |
| Secondary | |
| To evaluate the effect at 12 months of iptacopan on a composite renal endpoint, in reducing glomerular inflammation in the kidney and in improvement of patient-reported fatigue | Requirements of the composite renal endpoint are met if the eGFR and UPCR criteria are satisfied at the 12-month time point (both treatment arms)* Proportion of participants who achieved the composite renal endpoint at 12 months Change from baseline in total activity score in a renal biopsy at 12 months (both treatment arms) Change in total activity score in a renal biopsy from the 6 month visit to the 12 month visit in the placebo arm Change from baseline in the FACIT-Fatigue score at 12 months (both study treatment arms) Change in the FACIT-Fatigue score from the 6 month visit to the 12 month visit of the placebo arm |
| To evaluate the safety and tolerability of iptacopan during the 6-month open-label treatment period as well as the entire 12-month treatment period | Vital signs, ECGs, safety laboratory measurements, AEs, AESIs |
In this trial, proteinuria and eGFR were selected as surrogate endpoints of disease progression1. The investigators noted proteinuria is considered a marker of kidney damage and risk for progression to ESKD in other glomerular diseases12,13. Level of proteinuria also has a role in prediction of treatment effect in long term outcome in various chronic kidney diseases, and emerging data supports use of proteinuria as a surrogate endpoint in C3G1,10,14,15. In addition, eGFR is supported as a surrogate endpoint in other glomerular diseases12,16,17.
Benefits and limitations of the APPEAR-C3G trial design
Some benefits and limitations of the APPEAR-C3G trial design are described below1,11.
Benefits
- Use of a randomised, double-blind and placebo-controlled approach for the first 6 months of the trial
- Inclusion of quality-of-life assessment as part of the study endpoints
- Concomitant treatment with various supportive (e.g. ACEi or ARB) and other anti-proteinuric medications were permitted during the study, provided the dose is stable
- Randomisation was stratified according to whether or not participants are receiving corticosteroid and/or mycophenolic acid at randomisation
Limitations
- Small sample size – approximately 68 participants are planned for enrolment in the trial, with 34 each in the iptacopan and placebo arms; however, this may be considered reasonable in the context of a rare disease such as C3G, and noting a sample size calculation was used in the study design18
- The duration of the double-blind, randomised and placebo-controlled treatment period is limited to 6 months
- Eligibility for inclusion in the trial is limited to those with a recent biopsy-confirmed diagnosis of C3G (i.e. in the 12 months prior to enrolment), and people with more severe disease are excluded (as reflected by exclusion of those with rapidly progressive crescentic GN renal biopsy with interstitial fibrosis/tubular atrophy >50); these will be important to consider for context when interpreting the study’s results
Additionally, there is a lack of clarity in the Bomback et al. (2022) publication regarding the design and purpose of the run-in period, as only the duration was provided (i.e. up to 90 days). Lack of detail on the design and purpose of a run-in period, and any reasons for exclusion during this time, can preclude a meaningful assessment of any potential impact it may have on the validity of trial results19. More details will likely be provided in study protocol when it becomes publicly available, and/or when the study results are published.
When will the APPEAR-C3G trial be completed?
The APPEAR-C3G trial commenced in July 202111, and is still recruiting participants as of 7 July 202311. Based on details provided on clinicaltrials.gov, the estimated study completion date of the trial is April 202611.
Watch a video on the mechanism of action of iptacopan in C3G
Learn more about other investigational treatments for C3G in our independent CMKDs Learning Zone
View highlights from the 2023 World Congress of Nephrology
References
- Bomback AS, Kavanagh D, Vivarelli M, Meier M, Wang Y, Webb NJ, et al. Alternative Complement Pathway Inhibition With Iptacopan for the Treatment of C3 Glomerulopathy-Study Design of the APPEAR-C3G Trial. Kidney Int Rep. 2022;7(10):2150-2159.
- Schena FP, Nistor I. Epidemiology of IgA nephropathy: a global perspective. Presented at the Semin Nephrol 2018.
- Smith RJH, Appel GB, Blom AM, Cook HT, D'Agati VD, Fakhouri F, et al. C3 glomerulopathy - understanding a rare complement-driven renal disease. Nat Rev Nephrol. 2019;15(3):129-143.
- Meuleman MS, Grunenwald A, Chauvet S. Complement C3-targeted therapy in C3 glomerulopathy, a prototype of complement-mediated kidney diseases. Semin Immunol. 2022:101634.
- Heiderscheit AK, Hauer JJ, Smith RJH. C3 glomerulopathy: Understanding an ultra-rare complement-mediated renal disease. Am J Med Genet C Semin Med Genet. 2022;190(3):344-357.
- Andrighetto S, Leventhal J, Zaza G, Cravedi P. Complement and Complement Targeting Therapies in Glomerular Diseases. Int J Mol Sci. 2019;20(24).
- Fakhouri F, Schwotzer N, Golshayan D, Frémeaux-Bacchi V. The rational use of complement inhibitors in kidney diseases. Kidney Int Rep. 2022;7(6):1165-1178.
- National Institutes of Health US National Library of Medicine. Clinicaltrials.gov. https://clinicaltrials.gov/ct2/home. Accessed 12 January 2023.
- NCT03832114. Study on efficacy and safety of LNP023 in C3 glomerulopathy patients transplanted and not transplanted. Available at: https://clinicaltrials.gov/ct2/show/study/NCT03832114. Accessed 16 February 2023.
- Wong E, Nester CM, Cavero escribano T, Karras A, Lequintrec-Donnette M, Lighstone L, et al. Iptacopan, a novel oral complement factor B (FB) inhibitor, significantly reduces proteinuria and C3 deposit scores in native and transplanted kidneys C3 glomerulopathy (C3G) patients. Presented at the American Society of Nephrology 2021, 4 November 2021. Virtual. PO2536. Available at: https://www.asn-online.org/education/kidneyweek/2021/program-abstract.aspx?controlId=3638501. Accessed 16 February 2023.
- NCT04817618. Study of efficacy and safety of iptacopan in patients with C3 glomerulopathy (APPEAR-C3G). Available at: https://clinicaltrials.gov/ct2/show/NCT04817618. Accessed 17 July 2023.
- Kidney Disease: Improving Global Outcomes Diabetes Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Oct 2021.
- Levey AS, Gansevoort RT, Coresh J, Inker LA, Heerspink HL, Grams ME, et al. Change in Albuminuria and GFR as End Points for Clinical Trials in Early Stages of CKD: A Scientific Workshop Sponsored by the National Kidney Foundation in Collaboration With the US Food and Drug Administration and European Medicines Agency. Am J Kidney Dis. 2020;75(1):84-104.
- Wong E, Praga M, Nester C, Le Quintrec M, Daina E, Remuzzi G, et al. FC 036 Iptacopan (LNP023): A novel oral complement alternative pathway factor B inhibitor safely and effectively stabilises eGFR in C3 glomerulopathy. Nephrology Dialysis Transplantation. 2021;36(Supplement_1).
- Caravaca-Fontán F, Díaz-Encarnación M, Cabello V, Ariceta G, Quintana LF, Marco H, et al. Longitudinal change in proteinuria and kidney outcomes in C3 glomerulopathy. Nephrol Dial Transplant. 2022;37(7):1270-1280.
- Barratt J, Rovin B, Diva U, Mercer A, Komers R. Implementing the Kidney Health Initiative Surrogate Efficacy Endpoint in Patients With IgA Nephropathy (the PROTECT Trial). Kidney International Reports. 2019;4(11):1633-1637.
- Greene T, Ying J, Vonesh EF, Tighiouart H, Levey AS, Coresh J, et al. Performance of GFR Slope as a Surrogate End Point for Kidney Disease Progression in Clinical Trials: A Statistical Simulation. J Am Soc Nephrol. 2019;30(9):1756-1769.
- Billingham L, Malottki K, Steven N. Small sample sizes in clinical trials: a statistician's perspective. Clin Invest. 2012;2(7):655-657.
- Laursen DRT, Paludan-Müller AS, Hróbjartsson A. Randomized clinical trials with run-in periods: frequency, characteristics and reporting. Clin Epidemiol. 2019;11:169-184.
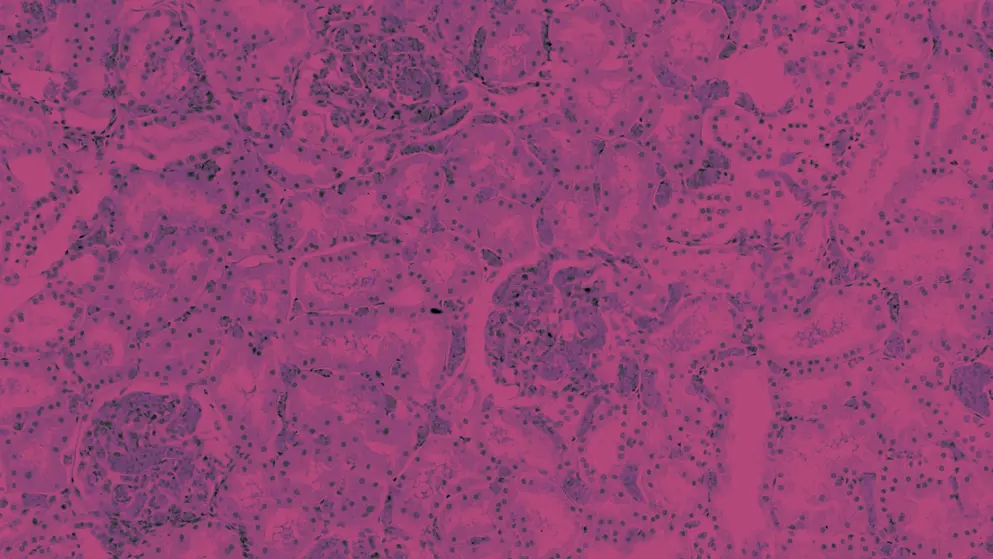
Histologic features associated with outcome in C3G and IG-MPGN
In this publication digest, learn about which histologic parameters in kidney biopsies were associated with clinical outcomes in a cohort of patients with C3 glomerulopathy (C3G) or idiopathic immunoglobulin membranoproliferative glomerulonephritis (Ig-MPGN).
Read more to learn about key findings from the study, its limitations and what the findings may mean in practice.
Association of histologic parameters with outcome in C3 glomerulopathy and idiopathic immunoglobulin-associated membranoproliferative glomerulonephritis
Source publication: Lomax-Browne HJ, Medjeral-Thomas NR, Barbour SJ, Gisby J, Han H, Bomback AS, et al. Clin J Am Soc Nephrol. 2022;17(7):994-10071
Both C3 glomerulopathy (C3G) and immunoglobulin-associated membranoproliferative glomerulonephritis (Ig-MPGN) are rare kidney diseases that are heterogenous in clinical presentation and outcomes1. With overlapping etiology and pathogenesis, both diseases involve abnormal complement C3 deposition and alternative complement pathway dysregulation1,2.
Within 10 years of diagnosis, 30–50% of adults with C3G or Ig-MPGN progress to kidney failure – however, it is difficult to identify which patients will have poor prognosis1
What did the investigators do?
This study investigated histological and clinical features associated with clinical outcome that could be used to develop outcome prediction tools for C3G/Ig-MPGN1, similar to that done in IgA nephropathy3,4.
Lomax-Browne and colleagues undertook a multicentre, centralised and retrospective review of native diagnostic kidney biopsies from a cohort of 156 adult and paediatric (<17 years of age) participants with C3G (n = 123) or idiopathic Ig-MPGN (n = 33). In the C3G cohort, 106 participants had C3 glomerulonephropathy (C3 GN) and 17 had dense deposit disease (DDD)1.
Histologic scoring was undertaken on biopsies using light microscopy. Immunofluorescence staining was extracted from biopsy reports, and electron microscopy was used to classify biopsies into the Ig-MPGN, C3 GN or DDD groups1. The investigators used the validated C3 glomerulopathy histologic index score to calculate biopsy activity and chronicity scores1. Linear regression, survival analysis and a Cox proportional hazards model were used to assess the relationship between histologic and clinical parameters with outcome1.
Study outcomes
The composite outcome was defined as1:
- the time to kidney failure (estimated glomerular filtration rate [eGFR] <15 ml/min/1.73m2, dialysis or transplantation),
- the first occurrence of doubling of the serum creatinine level from baseline (adults), or
- 30% reduction of eGFR (for paediatric patients)
Longitudinal proteinuria was also assessed across 75 months1.
Outcome-free survival and changes in proteinuria over 12 months were analysed in a subset of 75 participants with 2 years of follow-up data, which could be used to reliably determine whether they had stable or progressive disease1.
What did the investigators find?
Results indicated that eGFR and proteinuria at the time of biopsy, and cellular/fibrocellular crescents, segmental sclerosis and interstitial fibrosis/tubular atrophy (IFTA) scores were associated with risk of progression to kidney failure, using the composite outcome1
This was demonstrated by the following findings1:
- eGFR and proteinuria at the time of baseline biopsy were associated with outcome-free survival and higher risk of progression to the combined outcome (Table 1)
- a significant association between cellular/fibrocellular crescents, segmental sclerosis, IFTA scores and outcome-free survival (Figure 1)
- segmental sclerosis, cellular/fibrocellular crescents, IFTA were associated with higher risk of progression to the combined outcome (Table 1)
Table 1. Covariates of the risk to progression to the combined outcome event* (multivariable analysis; Adapted1). C3G, C3 glomerulopathy; eGFR, estimated glomerular filtration rate; HR, hazard ratio; Ig-MPGN, idiopathic immunoglobulin-associated membranoproliferative glomerulonephritis; IFTA, interstitial fibrosis/tubular atrophy. *Composite outcome defined as the time to kidney failure (eGFR <15 ml/min per 1.73m2, dialysis or transplantation), the first occurrence of doubling of the serum creatinine level from baseline (adults), or 30% reduction of eGFR (for paediatric patients)1.
| Clinical covariate | n | Unadjusted HR (95% CI) | |
| C3G cohort | All cohort (C3G + Ig-MPGN) |
||
| eGFR <45 ml/min/1.73m2 | All cohort = 53 C3G = 44 |
3.48 (1.57 to 7.68) | 3.08 (1.46 to 6.52) |
| Proteinuria <2g/day | All cohort = 88 C3G = 65 |
5.53 (1.83 to 16.76) | 5.14 (1.86 to 13.43) |
| Segmental sclerosis >25% | All cohort = 39 C3G = 34 |
6.42 (2.01 to 20.50) | 1.94 (0.82 to 4.56) |
| Cellular/fibrocellular crescent >25% | All cohort = 9 C3G = 8 |
2.48 (0.88 to 7.00) | 3.50 (1.46 to 8.41) |
| IFTA >50% | All cohort = 11 C3G = 10 |
2.44 (0.64 to 9.37) | 5.11 (1.49 to 17.45) |
Figure 1. Outcome-free survival by histologic score in the C3G cohort†‡ (Adapted1). C3G, C3 glomerulopathy; C3GN, C3 glomerulonephritis. *The combined/composite outcome was defined as time to kidney failure (eGFR <15 ml/min/1.73m2, dialysis or transplantation), the first occurrence of doubling of serum creatinine level from baseline (adults), or 30% reduction of eGFR (for paediatric patients). †Outcome-free survival and risk of progression to the combined event were based on the composite outcome1. ‡C3G cohort (n=118), includes 101 with C3GN and 17 with dense deposit disease1.
Benefits and limitations of the study
Benefits of the study include its use of a validated histologic score, analysis of histologic features that are routinely assessed at kidney biopsy1, and use of a centralised pathology review of all biopsies1.
Limitations of this study included:
- the use of a retrospective cohort, in which data were not available for all participants, noting 2-year follow-up data was unavailable for over half of the cohort (81/156)
- limited details provided on the recruitment method for the initially recruited cohort of 193 participants, the dates of recruitment and approximate dates of diagnosis
- participants were mostly white (75%), with few participants of Asian, Black or other ethnicity
- a lack of comprehensive complement genetic data
- limited detail on data points used for statistical significance calculations
In addition, there was potential for confounding of results from:
- pooling of data for adult and paediatric populations, considering prognosis may be more favourable in paediatric patients compared to adults5-7
- differences in treatment and management across multiple sites (UK, US, Australia), noting results were not stratified to account for these potential confounders
The authors noted potential confounding from a lack of uniform treatment across sites may have been mitigated by the lack of specific disease-modifying treatments1. Although baseline characteristics showed variation in immunosuppressant treatments across groups, the study’s univariate analysis showed immunosuppression use was not strongly associated with risk of progression to the combined event, or with differences in histology scores over time1.
Key learnings from this study
The results of this study indicated that IFTA, cellular/fibrocellular crescents and segmental sclerosis were histologic determinants of risk of progression to kidney failure, and could be incorporated in risk prediction tools to stratify C3 glomerulopathy and Ig-MPGN at diagnosis1
Lomax-Browne and colleagues suggested the development of such tools for C3G/Ig-MPGN may help to identify patients with poor prognosis, and may also improve patient stratification in clinical trials1.
However, these histologic determinants remain to be validated in a larger cohort, and a risk prediction tool for patients with C3G or Ig-MPGN based on these determinants also remains to be developed and validated.
Explore types of CMKDs, their prevalence, impact and key aspects of their clinical presentation
View highlights from the 2023 World Congress of Nephrology
References
- Lomax-Browne HJ, Medjeral-Thomas NR, Barbour SJ, Gisby J, Han H, Bomback AS, et al. Association of histologic parameters with outcome in C3 glomerulopathy and idiopathic immunoglobulin-associated membranoproliferative glomerulonephritis. Clin J Am Soc Nephrol. 2022;17(7):994-1007.
- Heiderscheit AK, Hauer JJ, Smith RJH. C3 glomerulopathy: Understanding an ultra-rare complement-mediated renal disease. Am J Med Genet C Semin Med Genet. 2022;190(3):344-357.
- Barbour SJ, Coppo R, Zhang H, Liu ZH, Suzuki Y, Matsuzaki K, et al. Evaluating a New International Risk-Prediction Tool in IgA Nephropathy. JAMA Intern Med. 2019;179(7):942-952.
- Barbour SJ, Espino-Hernandez G, Reich HN, Coppo R, Roberts IS, Feehally J, et al. The MEST score provides earlier risk prediction in lgA nephropathy. Kidney Int. 2016;89(1):167-175.
- Kirpalani A, Jawa N, Smoyer WE, Licht C. Long-Term Outcomes of C3 Glomerulopathy and Immune-Complex Membranoproliferative Glomerulonephritis in Children. Kidney Int Rep. 2020;5(12):2313-2324.
- Michels MAHM, Wijnsma KL, Kurvers RAJ, Westra D, Schreuder MF, van Wijk JAE, et al. Long-term follow-up including extensive complement analysis of a pediatric C3 glomerulopathy cohort. Pediatric Nephrology. 2022;37(3):601-612.
- Zahir Z, Wani AS, Gupta A, Agrawal V. Pediatric C3 glomerulopathy: a 12-year single-center experience. Pediatric Nephrology. 2021;36(3):601-610.
Nomograms to predict kidney survival
Read our publication digest to learn about the development and validation of a nomogram to predict kidney survival at baseline in people with C3 glomerulopathy (C3G). Learn about the study rationale and aims, and:
- explore aspects of the study design in detail
- consider the benefits and limitations of the study
- identify the study outcomes
Development and validation of a nomogram to predict kidney survival at baseline in people with C3 glomerulopathy
Source publication: Caravaca-Fontán F, et al. Clin Kidney J. 2022;15(9):1737–17461
C3 glomerulopathy (C3G) is a rare kidney disorder characterised by abnormal activation of the complement system, leading to glomerular inflammation and renal damage2,3. Determining the prognosis and predicting kidney survival in people with C3G is essential for optimising treatment strategies and improving patient outcomes3.
Caravaca-Fontán et al. aimed to develop and validate a nomogram – a predictive tool – to estimate kidney survival at baseline (time of C3G diagnosis) in people with C3G1.
The development and validation of a nomogram to predict kidney survival at baseline in people with C3G represents a valuable tool for personalised prognostication in this rare kidney disorder1
What did the investigators do?
The study utilised a retrospective cohort of people diagnosed with C3G, with data collected from multiple medical centres in Spain1. The primary outcome of interest was kidney failure, defined as an estimated glomerular filtration rate (eGFR) of <15 mL/min/1.73 m2, or the need for dialysis or initiation of kidney replacement therapy1.
The researchers used a least absolute shrinkage and selector option (LASSO) regression model, in which 10 variables were included, to screen for the main predictors of kidney failure. Variables included were1:
- age at diagnosis
- gender
- presence of complement pathogenic variants
- anti-complement antibodies
- serum albumin level
- serum C3 level
- baseline eGFR
- proteinuria
- total activity (a disease activity score generated from histological findings on biopsy)
- chronicity score (generated from histological findings on biopsy)
What were the main findings?
A total of 115 people with C3G were included in the study cohort and subsequently divided into a training group (n=87) and a validation group (n=28). Among them, 46 reached kidney failure in the median follow-up of 49 months. The rates of kidney survival are shown in Table 11.
Table 1. Kidney survival rates at 1, 2, 5 and 10 years post-C3G diagnosis1.
| Year | Survival probability rate (%) |
| 1 | 80 |
| 2 | 75 |
| 5 | 61 |
| 10 | 24 |
Of the 10 variables included in the LASSO model, baseline eGFR, proteinuria and chronicity score were identified as independent predictors of kidney failure and incorporated into a Cox regression to build the nomogram, which predicts the likelihood of kidney failure or probability of kidney survival at 1, 2, 5 and 10 years (Figure 1)1.
Figure 1. Nomogram for the prediction of kidney failure at 1, 2, 5 and 10 years1. Image licensed under CC-BY-NC 4.0 from Caravaca-Fontán F et al. Clin Kidney J. 2022;15(9):1737–1746.
To use the nomogram, identify each patient-specific variable, align it with the 'points' axis to find the corresponding value and add the three values to determine the total points. From the 'total points' axis, draw a line downwards from the patient’s total score to 1, 2, 5 and 10 years, to determine risk of kidney failure/probability of kidney survival at these time points1. For example, a baseline eGFR of 65 mL/min/1.73 m2, proteinuria of 2 g/day and total chronicity score of three would translate to a total of 87 points (45 + 12 + 30), which predicts kidney survival of 94% at 1 year, 90% at 2 years, 77% at 5 years and 72% at 10 years1.
Internal validation of the nomogram was based on discrimination and calibration. The concordance index (C-index) was 0.860 (95% confidence interval, 0.834–0.887). Calibration plots also demonstrated optimal correlation between the predicted and the observed outcomes1.
Benefits and limitations
The nomogram exhibited good discrimination and calibration abilities in both the training and validation cohorts1. Its predictive performance was further evaluated using measures such as the C-index and calibration plots, which demonstrated its reliability and accuracy1.
The development and validation of a nomogram to predict kidney survival at baseline in people with C3G is a significant advancement in the field of renal medicine. The nomogram provides a practical and user-friendly tool for clinicians to estimate the risk of progression to kidney failure and to aid in treatment decision-making1.
Despite its valuable contributions, a limitation of the study was the relatively small cohort size, which may affect the generalisability of the nomogram's performance in larger and more diverse populations1.
Independent predictors of kidney failure – baseline eGFR, proteinuria and chronicity – were identified and used to construct a validated, user-friendly tool for predicting kidney survival in people diagnosed with C3G1
Key learning points
By identifying the level of risk at the time of C3G diagnosis, clinicians can implement the appropriate therapeutic strategy for a given person to potentially delay or prevent the development of renal failure1,4.
Inclusion of various clinical and laboratory parameters in the nomogram highlights the complex nature of C3G and the importance of a comprehensive approach to prognosis assessment1.
Learn more about other investigational treatments for C3G in our independent CMKDs Learning Zone
Explore types of CMKDs, their prevalence, impact and key aspects of their clinical presentation
View highlights from the 2023 World Congress of Nephrology
References
- Caravaca-Fontán F, Rivero M, Cavero T, Díaz-Encarnación M, Cabello V, Ariceta G, et al. Development and validation of a nomogram to predict kidney survival at baseline in patients with C3 glomerulopathy. Clin Kidney J. 2022;15(9):1737-1746.
- Schena FP, Esposito P, Rossini M. A narrative review on C3 glomerulopathy: A rare renal disease. Int J Mol Sci. 2020;21(2):525.
- Smith RJH, Appel GB, Blom AM, Cook HT, D'Agati VD, Fakhouri F, et al. C3 glomerulopathy - understanding a rare complement-driven renal disease. Nat Rev Nephrol. 2019;15(3):129-143.
- Anwar IJ, DeLaura I, Ladowski J, Gao Q, Knechtle SJ, Kwun J. Complement-targeted therapies in kidney transplantation—insights from preclinical studies. Frontiers in Immunology. 2022;13:984090.

