IgA nephropathy (IgAN)
In this section
What is IgA nephropathy?
About IgA nephropathy
Immunoglobulin A nephropathy (IgAN) is the most common form of glomerulonephritis worldwide1,2 and a leading cause of kidney failure3. IgAN is an autoimmune kidney disease caused by deposition of galactose-deficient IgA1-containing immune complexes in the glomerular mesangium, leading to inflammation and kidney injury3-5.
IgAN is a highly heterogenous disease, with variation across geographic regions and populations in2,3,6,7:
- incidence, prevalence and sex distribution
- clinical presentation and progression
- pathogenic initiating factors
- treatment response
Without effective treatment, IgAN can lead to irreversible worsening of kidney function7, and is associated with high morbidity and mortality3,7.
Incidence, prevalence and burden of IgA nephropathy
The incidence of IgAN is at least 2.5 per 100,000 per population per year1, with peak incidence at 10–30 years of age3,8.
The prevalence of IgAN shows marked variation across geographic regions and ethnic groups6, and is much higher in people from East Asia, compared with those in North America and Europe2,3. Of primary glomerulonephritis cases, IgAN accounts for approximately7:
- 10–20% in the United States
- 20–30% in some European countries
- 40–50% in developed Asian countries
However, prevalence data for IgAN does not encompass subclinical IgAN3, and is complicated by the need for biopsy-based diagnosis9. Geographical variability in prevalence may be influenced by different health screening policies and biopsy practices between regions, and genetic susceptibility3.
Although its clinical course is highly variable3, IgAN is associated with an increased risk of mortality, and a 6–10 year reduction in life expectancy from progression to kidney failure3,7.
Approximately 20–40% of people with IgAN will have reached kidney failure within 20 years after diagnosis3
As IgAN is a major cause of kidney failure in young adults, the worsening renal impairment from this disease has been associated with loss of labour force participation and a significant social burden7.
Signs and symptoms of IgA nephropathy
The clinical presentation of IgAN is variable, ranging from asymptomatic microscopic haematuria to sustained proteinuria and rapidly declining kidney function6.
The hallmark clinical feature of IgAN is episodic, visible (macroscopic) haematuria, due to red blood cells passing through the glomeruli into the urinary space3. In children and young adults, this is often accompanied by febrile illness3. In adults, microscopic haematuria is often observed, with or without proteinuria3.
IgAN should be suspected in young people with a history of macroscopic haematuria, especially if accompanied by febrile illness, and in cases of asymptomatic haematuria and/or proteinuria3
Evidence suggests the clinical presentation of IgAN can vary by geographical region6. In particular, people with IgAN from Asia have been reported to:
- present with more severe clinical signs and symptoms, and a higher risk of disease progression, compared with people with IgAN from Europe6
- have a more rapid rate of kidney function decline, compared with other regions of the world6
Pathophysiology of IgA nephropathy
The pathogenesis of IgAN involves dysregulated IgA production1, resulting in deposition of galactose-deficient IgA1-containing immune complexes in the glomerular mesangium9,10.
Although the precise mechanism through which IgA becomes dysregulated remains unclear1, the pathogenesis of IgAN is widely accepted to follow the four-hit process (Figure 1) that starts with abnormal production of galactose-deficient IgA15,7,11. Ultimately, this results in accumulation of immune complexes in the glomerular mesangium, and leads to inflammation, progressive scarring and impairment of kidney function3.
Figure 1. The four-hit hypothesis for IgAN pathogenesis11-15 (Adapted14 under Creative Commons License CC-BY-4.0). High blood levels of Gd-IgA1 (Hit 1) and production of autoantibodies specific for Gd-IgA1 (Hit 2) lead to formation of pathogenic circulating immune complexes (Hit 3)3,11, which accumulate in glomeruli and induce kidney injury (Hit 4)3,11,15.
Through an evolving understanding of IgAN, it is now recognised that its pathophysiology also involves the immune response, complement activation, mucosal immunity, kidney inflammation and autophagy7.
Genetic factors may also influence susceptibility to IgAN, which may account for some of the geographic and ethnic variation in prevalence of the disease7.
The role of complement in IgA nephropathy
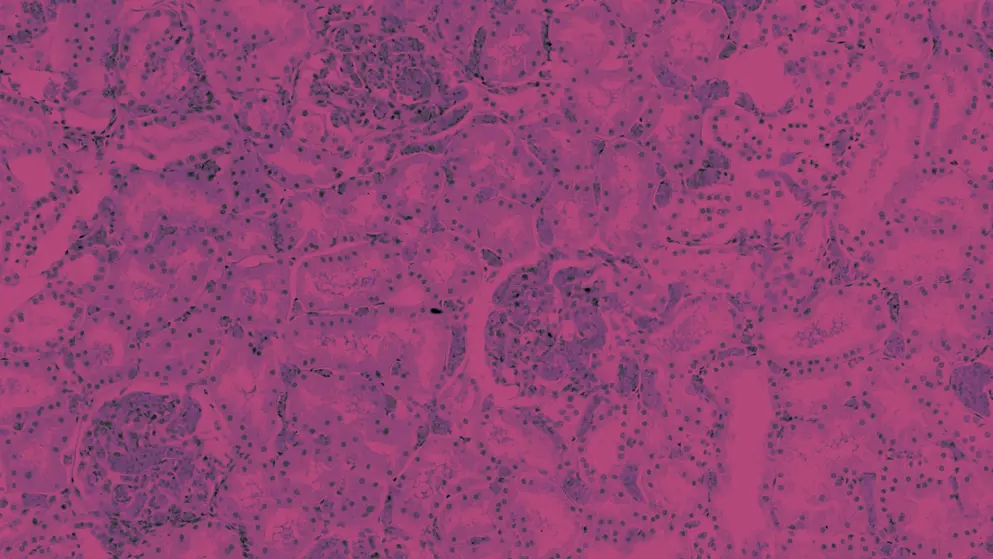
A combination of histological, genetic and clinical data indicate that activation of the alternative and lectin pathways of the complement cascade are involved in the pathophysiology of IgAN3. This complement activation and subsequent deposition of complement components in the kidney (Figure 2) are thought to initiate and/or amplify glomerular inflammation and kidney injury14.
Figure 2. Local activation of the alternative and lectin complement pathways and renal deposition of complement components in IgAN3,5,14,16-18 (Adapted14 under Creative Commons License CC BY 4.0). Gd-IgA1, galactose-deficient IgA1; IgAN, IgA nephropathy; MBL, mannose-binding lectin; MASP, MBL-associated serine protease.
The most frequently observed complement component deposits in IgAN biopsies are C3 (colocalised with IgA in >90% of IgAN biopsies3,6), Factor H (69–85%) and C5b9 (75%)3.
It is thought that glomerular deposition of galactose-deficient IgA1 immune complexes can trigger complement activation via the alternative pathway, leading to renal deposition of complement components19
Evidence suggests a possible association between renal complement deposition in IgAN and disease severity and/or prognosis. For example, mannose-binding lectin (MBL) or C4d deposition have been associated with worse prognosis5, while C5a deposition has been correlated with proteinuria and pathological grade in IgAN16.
Particular complement components appear to be associated with IgAN severity in specific geographic locations and ethnic groups6. For example, serum MBL levels have been associated with IgAN severity in Chinese, but not non-Chinese populations6. The authors considered this may suggest that differences in complement dysregulation could contribute to the more severe clinical patterns and pathology observed in people with IgAN from Asia6.
Genetic variants in complement genes have also been associated with outcomes in IgAN14. Risk variants in the MBL2 gene have been associated with an increased risk of IgAN progression20, while a common deletion within the Factor H gene locus may be protective against IgAN14. This deletion results in loss of the FHR1 and FHR3 genes, while leaving the gene for Factor H intact; each copy of the deletion was reported to reduce the risk of IgAN by almost 40% 14,21,22. It is thought that this protective effect may arise from reduced competition of Factor H-related proteins with Factor H, which may promote inhibition rather than activation, possibly reducing inflammation14.
While complement activation, deposition and genetic changes have been associated with various aspects of IgAN, the precise mechanisms through which the lectin pathway and alternative pathway are acivated in IgAN remain to be elucidated5. Further research will help to better characterise the mechanisms of complement activation in IgAN, and shed more light on their contribution to disease pathophysiology17.
Challenges in IgAN management
Effective and well-tolerated disease-modifying agents that target the underlying pathophysiology of IgAN are greatly needed3,7,23, as management of IgAN has been largely limited to supportive measures7,24. These supportive measures include the use of antihypertensive agents to control blood pressure and reduce proteinuria, and immunosuppressants7,24. However, treatment response is variable, and up to 40% of patients with IgAN still progress to kidney failure within 20 years of diagnosis3,5,7.
A targeted-release form of the corticosteroid budesonide was granted accelerated approval by the US Food and Drug Administration (FDA) in 202125,26 and by the European Medicines Agency (EMA) in 202227, for treatment of IgAN. This formulation delivers a delayed release of budesonide to the distal ileum, suppressing local immune cell activity, including Gd-IgA1-producing cells that cause immune complex formation in IgAN23. Results of clinical trials have demonstrated a reduction in proteinuria and stablisation of kidney function in patients with IgAN who were treated with this formulation23,28. The approval of this medicine has strengthened interest in targeting the underlying pathogenesis of IgAN23.
As our understanding of the IgAN pathogenesis evolves, further new treatment approaches are being investigated in clinical trials, including those that target the complement cascade and other immunological pathways that contribute to the disease3.
Are you interested in more information on diagnosis, risk prediction, treatment, unmet needs and investigational treatments for IgAN? More content is coming soon to this learning zone. Stay tuned for further updates
Learn about complement-mediated kidney diseases, their burden and impact
References
- Storrar J, Chinnadurai R, Sinha S, Kalra PA. The epidemiology and evolution of IgA nephropathy over two decades: A single centre experience. PLoS One. 2022;17(9):e0268421.
- Suzuki Y, Monteiro RC, Coppo R, Suzuki H. The phenotypic difference of IgA nephropathy and its race/gender-dependent molecular mechanisms. Kidney360. 2021;2(8):1339-1348.
- Rajasekaran A, Julian BA, Rizk DV. IgA Nephropathy: An Interesting Autoimmune Kidney Disease. Am J Med Sci. 2021;361(2):176-194.
- Lai KN. Future directions in the treatment of IgA nephropathy. Nephron. 2002;92(2):263-270.
- Le Stang MB, Gleeson PJ, Daha MR, Monteiro RC, van Kooten C. Is complement the main accomplice in IgA nephropathy? From initial observations to potential complement-targeted therapies. Mol Immunol. 2021;140:1-11.
- Zhang H, Barratt J. Is IgA nephropathy the same disease in different parts of the world? Semin Immunopathol. 2021;43(5):707-715.
- Huang X, Xu G. An update on targeted treatment of IgA nephropathy: an autoimmune perspective. Front Pharmacol. 2021;12:715253.
- Barratt J, Feehally J. IgA Nephropathy. J Am Soc Nephrol. 2005;16(7):2088-2097.
- Rawla P, Limaiem F, Hashmi MF. IgA nephropathy. Treasure Island (FL): StatPearls Publishing; 2022.
- Suzuki H. Biomarkers for IgA nephropathy on the basis of multi-hit pathogenesis. Clin Exp Nephrol. 2019;23(1):26-31.
- Suzuki H. Biomarkers for IgA nephropathy on the basis of multi-hit pathogenesis. Clin Exp Nephrol. 2019;23(1):26-31.
- Magistroni R, D'Agati VD, Appel GB, Kiryluk K. New developments in the genetics, pathogenesis, and therapy of IgA nephropathy. Kidney Int. 2015;88(5):974-989.
- Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, et al. The pathophysiology of IgA nephropathy. J Am Soc Nephrol. 2011;22 10:1795-1803.
- Poppelaars F, Faria B, Schwaeble W, Daha MR. The Contribution of Complement to the Pathogenesis of IgA Nephropathy: Are Complement-Targeted Therapies Moving from Rare Disorders to More Common Diseases? Journal of Clinical Medicine. 2021;10(20):4715.
- Lai KN, Tang SC, Schena FP, Novak J, Tomino Y, Fogo AB, et al. IgA nephropathy. Nat Rev Dis Primers. 2016;2:16001.
- Liu L, Zhang Y, Duan X, Peng Q, Liu Q, Zhou Y, et al. C3a, C5a renal expression and their receptors are correlated to severity of IgA nephropathy. J Clin Immunol. 2014;34(2):224-232.
- Medjeral-Thomas NR, Cook HT, Pickering MC. Complement activation in IgA nephropathy. Semin Immunopathol. 2021;43(5):679-690.
- Rizk DV, Maillard N, Julian BA, Knoppova B, Green TJ, Novak J, et al. The emerging role of complement proteins as a target for therapy of IgA nephropathy. Front Immunol. 2019;10:504.
- Zipfel PF, Wiech T, Gröne HJ, Skerka C. Complement catalyzing glomerular diseases. Cell Tissue Res. 2021;385(2):355-370.
- Ouyang Y, Zhu L, Shi M, Yu S, Jin Y, Wang Z, et al. A rare genetic defect of MBL2 increased the risk for progression of IgA nephropathy. Front Immunol. 2019;10:537.
- Gharavi AG, Kiryluk K, Choi M, Li Y, Hou P, Xie J, et al. Genome-wide association study identifies susceptibility loci for IgA nephropathy. Nature Genetics. 2011;43(4):321-327.
- Kiryluk K, Li Y, Sanna-Cherchi S, Rohanizadegan M, Suzuki H, Eitner F, et al. Geographic Differences in Genetic Susceptibility to IgA Nephropathy: GWAS Replication Study and Geospatial Risk Analysis. PLOS Genetics. 2012;8(6):e1002765.
- Maixnerova D, El Mehdi D, Rizk DV, Zhang H, Tesar V. New treatment strategies for IgA nephropathy: targeting plasma cells as the main source of pathogenic antibodies. J Clin Med. 2022;11(10):2810.
- Kidney Disease: Improving Global Outcomes Diabetes Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Oct 2021.
- US Food and Drug Administration, 2021. FDA approves first drug to decrease urine protein in IgA nephropathy, a rare kidney disease [press release]. Available at: https://www.fda.gov/drugs/fda-approves-first-drug-decrease-urine-protein-iga-nephropathy-rare-kidney-disease#:~:text=FDA%20has%20granted%20accelerated%20approval,risk%20of%20rapid%20disease%20progression. Accessed 20 April 2023.
- PR Newswire, 2021. FDA grants Calliditas Therapeutics accelerated approval of TARPEYO™ (budesonide) to Reduce Proteinuria in IgA Nephropathy [press release]. Available at: https://www.prnewswire.com/news-releases/fda-grants-calliditas-therapeutics-accelerated-approval-of-tarpeyo-budesonide-to-reduce-proteinuria-in-iga-nephropathy-301445918.html. Accessed 20 April 2023.
- European Medicines Agency. Kinpeygo (budesonide). https://www.ema.europa.eu/en/medicines/human/EPAR/kinpeygo. Accessed 20 April 2023.
- Barratt J, Lafayette R, Kristensen J, Stone A, Cattran D, Floege J, et al. Results from part A of the multi-center, double-blind, randomized, placebo-controlled NefIgArd trial, which evaluated targeted-release formulation of budesonide for the treatment of primary immunoglobulin A nephropathy. Kidney International. 2023;103(2):391-402.
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
