Complement in kidney disease
What are complement-mediated kidney diseases?
What are CMKDs?
Complement-mediated kidney diseases (CMKDs) is a collective term that refers to kidney diseases in which complement dysregulation is considered to cause or play a key role in their pathophysiology, contributing to kidney inflammation and injury 1-4.
Dr Edwin Wong, a consultant nephrologist from the UK, discusses the biggest obstacles and unmet needs patients face when diagnosed with CMKDs, particularly for those with C3 glomerulopathy (C3G).
The complement system is a key component of the innate immune system and is part of first-line defence against invading pathogens such as bacteria and viruses5,6. It triggers inflammation, phagocytosis and lysis of target cells2,5,7-9.
However, dysregulation of the complement system can result in its overactivation and cause harm to host tissues, leading to complement-mediated pathologies2,5,10. Complement overactivation has been implicated in a range of diseases5,6, and the kidney is particularly susceptible to damage from complement overactivation2,5.
Dysregulation of the complement system is considered the main driver of two types of CMKDs – C3 glomerulopathy (C3G) and atypical hemolytic uremic syndrome (aHUS)1,2,11
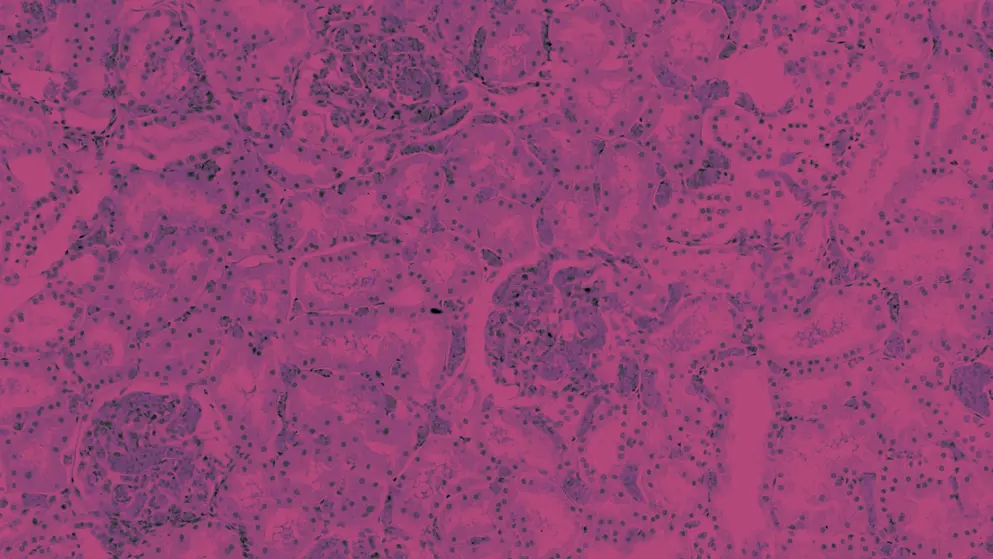
Evidence also suggests complement dysregulation contributes to the pathophysiology of other CMKDs such as IgA nephropathy (IgAN), immune complex-mediated membranoproliferative glomerulonephritis (IC-MPGN) and primary membranous nephropathy (MN) (Figure 1)1,2,5,11-14.
Figure 1. Types of CMKDs, other kidney conditions with complement involvement, and some typical findings on kidney biopsy1,2,4,5,11-13,15-19. ANCA, antineutrophil cytoplasmic antibody; GBM, glomerular basement membrane antibody; IC-MGPN, immune complex-mediated membranoproliferative glomerulonephritis; Ig, immunoglobulin; IgA1, immunoglobulin A1. *IC-MPGN is also known as immune complex-mediated glomerulonephritis (ICGN)20. †Although the predominant IgG subclass in membranous nephropathy (IgG4) is not considered to activate complement12, research suggests altered IgG4 can promote activation of the lectin complement pathway21, and activation of the alternative pathway has been implicated22. Note: This figure is not a comprehensive list of all kidney diseases in which complement dysregulation has been implicated.
Prevalence, impact and burden of CMKDs
CMKDs are chronic and progressive diseases1,2,4 and can have a devastating impact on patients23. They can progress to kidney failure1,23, requiring dialysis or transplantation2, and have been associated with an increased risk of mortality24-26. The incidence, prevalence and prognosis associated with CMKDs are summarised in Table 1.
Table 1. Incidence, prevalence and prognosis for C3G, aHUS, MN and IgAN‡1,2,4,5,11,15,16,27-30. aHUS, atypical hemolytic uremic syndrome; C3G, C3 glomerulopathy; IgAN, IgA nephropathy; MN, membranous nephropathy. *In Europe and the US29,30; †Worldwide18; ‡Incidence and prevalence data for immune complex-membranoproliferative glomerulonephritis were not available.
| Disease | Incidence and prevalence | Prognosis/outcomes |
| C3G | Incidence: 1–3 cases/million/year Prevalence: 0.2–5/million* Often diagnosed in children and young adults; median age at diagnosis is 22 years |
• Progression to kidney failure within 10 years in 30–50% of patients • High risk of recurrence after kidney transplantation |
| aHUS | Incidence: 0.23–1.9/million/year Prevalence: ~2–10/million/year Affects adults and children, more prevalent in children aged 0–4 years |
• Progression to kidney failure in ~50% of patients • Overall mortality rate of ~25%, but prognosis has improved since the introduction of eculizumab |
| IgAN | Incidence: 0.2–2.8/100,000/year Prevalence: Geographical variation (higher in Far East Asia, lower in Europe and Africa) Peak incidence between 10–30 years of age |
• Progression to kidney failure within 20 years in up to 40% of patients |
| MN | Incidence: 8–10/million/year† Prevalence: Data unavailable Most common over 40 years of age |
• Progression to kidney failure within 5–10 years in up to 40% of patients |
An overview of the complement system in health and disease
The role of complement in the immune system
The complement system is a crucial component of the innate immune system and is our first-line defence against invading pathogens such as bacteria and viruses5,6. Complement plays a key role in triggering the inflammatory response5, aids in priming and recruitment of immune cells, elimination of pathogens, and clearance of damaged cells and tissues from the body5,6,9. The complement system also helps to maintain cell homeostasis6, and contributes to protection against abnormal self-derived components6,9. It can also influence other physiological processes and systems, including coagulation, angiogenesis, tissue development and repair, and lipid metabolism5.
The complement system can be activated by pathogenic surface patterns or factors5. Once activated, the functions of the complement system are achieved by sequential activation of a cascade containing over 40 activating, amplifying or regulatory effectors2,5.
The products from complement cascade activation induce inflammation, act as chemoattractants for immune cells, tag target cells for elimination (opsonisation), and induce lysis of pathogenic, abnormal or diseased cells2,5,7-9
A closer look at the complement system
Activation of the complement cascade can occur via the classical, lectin and alternative activation pathways5. Each of these three major pathways is triggered by distinct pathogenic surface patterns or factors5.
- The classical pathway is activated by antigen–antibody reactions, viral or Gram-negative bacterial envelopes, C-reactive protein or apoptotic cells5
- The lectin pathway is activated by exposure to and binding of mannose residues on bacterial, fungal or viral pathogens5
- The alternative pathway remains constantly active at low levels5,9,33, acting as a surveillance system that monitors for pathogens and debris9
An overview of these complement activation pathways and their downstream biological effects is provided in Figure 2.
Figure 2. Pathways of complement cascade activation and their biological relevance2,5,7,8,34-37 (Adapted5 under Creative Commons license CC BY 4.0). This figure highlights the three different pathways for activation (blue) of the complement cascade: the classical, lectin and alternative. The alternative pathway is constitutively active at a low level via spontaneous hydrolysis of C3 (tick-over) to enable rapid amplification of the signal2,5,34. Each of the three pathways initiate formation a C3 convertase, and then undergo common amplification (orange) and terminal (red) stages2,5,34. The products of the complement cascade trigger downstream biological effects for immune defence and immune system homeostasis, including inflammation, opsonisation (tagging for phagocytosis) and lysis of target cells5,34. IgG, immunoglobulin G; IgM, immunoglobulin M; LPS, lipopolysaccharide. Note: This figure is intended as a simplified schematic representation, not a comprehensive overview of all components and consequences of complement cascade activation.
After activation, the key event in the cascade is amplification of the process via formation of C3 convertase2. C3 convertase creates a positive feedback amplification loop1, mainly driven by the alternative pathway1,2, leading to production of C3a and C3b2. C3a induces an inflammatory response38, and C3b triggers opsonisation of target cells39.
Subsequently, this leads to formation of C5 convertase and activation of the terminal pathway, producing components C5a and C5b2. C5a induces an inflammatory response and acts as a chemoattractant for immune cells5, while C5b drives the formation of a membrane attack complex (MAC) that lyses target cells2.
Regulation of the complement system
To prevent excessive complement activation and injury to self, the activity of the complement cascade is tightly regulated by soluble and membrane-bound inhibitory proteins2,6.
Strict regulation of alternative pathway activation and the amplification loop are particularly important in preventing complement overactivation and injury to self1
Inhibitory proteins that influence activity of the complement cascade include Factor B, Factor D, Factor H, Factor I and CD461,2. Failure of these regulatory mechanisms to limit complement activation can drive complement-mediated pathologies, such as complement-mediated kidney diseases (CMKDs)2.
Dysregulation of the complement system
When control of the complement system becomes dysfunctional, overactivation of the complement cascade can cause damage to host tissues, uncontrolled inflammation and complement-mediated pathologies2,5,10. Dysregulation of the complement system can arise from genetic causes, including gain-of-function mutations in activators and loss-of-function mutations in complement pathway inhibitors2. In other cases, complement dysregulation can be acquired, such as after infections and/or from production of autoantibodies2.
Dysregulation of complement contributes to pathogenesis across a range of diseases, including paroxysmal nocturnal haemoglobinuria, systemic lupus erythematosus, rheumatoid arthritis and various kidney diseases5,6.
The kidney is particularly susceptible to damage from complement dysfunction and overactivation2,5. Potential reasons for this include:
- The kidney’s key role in haemofiltration, leaving it prone to deposition of circulating immune complexes, which can trigger inflammation and immune cell infiltration5
- Lower baseline levels of complement regulators in the kidney5
Indeed, complement activation has been implicated in a range of kidney diseases including C3 glomerulopathy (C3G), atypical hemolytic uremic syndrome (aHUS), membranous nephropathy (MN) and IgA nephropathy (IgAN)1,12.
Pathophysiology of CMKDs
While the strongest causal evidence for complement dysregulation in kidney disease pathophysiology exists for C3 glomerulopathy (C3G) and atypical hemolytic uremic syndrome (aHUS), evidence supports a role for complement activation in the pathophysiology of other kidney diseases. These include1,2,5,11,12,14:
- IgA nephropathy (IgAN)
- immune complex-mediated membranoproliferative glomerulonephritis (IC-MPGN)
- membranous nephropathy (MN)
Join Dr Carla Nester as she explores the role of complement dysregulation in C3G and IgAN.
To date, evidence supports inclusion of C3G, aHUS, IgAN, IC-MPGN and primary MN under the umbrella term ‘complement-mediated kidney diseases (CMKDs)’12-14,40. The role of complement dysregulation in the pathophysiology of CMKDs is supported by clinical, pathological, genetic, animal and experimental studies12. Key clinical evidence on the role of complement dysregulation and renal deposition in the pathogenesis of C3G, aHUS, IgAN and MN is summarised in Table 212.
Table 2. The role of complement dysregulation and deposition in the pathogenesis of C3G, aHUS, IgAN, MN and IC-MPGN1,2,4,5,11,13,22,28,41-44. aHUS, atypical hemolytic uremic syndrome; CFHRs, complement factor H-related proteins; C3G, C3 glomerulopathy; IC-MPGN, immune complex-mediated membranoproliferative glomerulonephritis; Ig, immunoglobulin; IgAN, IgA nephropathy; IgA1, immunoglobulin A1; IgG, immunoglobulin G; IgG4, immunoglobulin 4; MASP-1, MBL-associated serine protease 1; MBL, mannose-binding lectin; MN, membranous nephropathy; TMA, thrombotic microangiopathy.
| Disease | Involvement of complement in pathogenesis |
| C3G | • Dysregulation of the alternative complement pathway is considered the main driver of disease o Can be genetic or acquired o Autoantibodies to C3 and C5 convertases are most common • C3, C3 convertase implicated o Activated C3 fragments (including C3b, iC3b, C3dg and C3d) are deposited in the glomerular basement membrane, leading to: - disrupted membrane function - an inflammatory response - glomerular damage • C5/C5 convertase axis also implicated in phenotype and severity of C3G |
| aHUS | • Dysregulation of the alternative complement pathway is considered the primary driver of disease o Loss of control of the alternative C3 convertase leads to complement overactivation, causing endothelial dysfunction in small blood vessels and TMA o C5 activation is a downstream consequence • Complement dysregulation can be hereditary or acquired and can involve: o Deficiencies in, or autoantibodies to, alternative pathway regulatory proteins (e.g. Factor H, Factor I, CD46) o Gain-of-function mutations in activator proteins (C3, Factor B) in the complement cascade |
| IgAN | • An immune-complex mediated disease, with a multi-hit theory of pathogenesis involving IgA and autoantibodies o Glomerular deposition of immune complexes (containing altered IgA1 and autoantibodies) leads to kidney inflammation and injury o Complement activation plays a role in IgAN pathophysiology - Alternative and lectin complement pathways are involved in the pathogenesis and severity of IgAN - Mechanism of complement activation by Igs remains speculative • Co-deposition of complement proteins with IgA deposits contributes to kidney injury (e.g. C3 [common], C5b9 [75%], C4d, MBL, MASP-1, Factor H, CFHRs 1–5, properdin) o Complement co-deposition has been associated with increased disease severity and/or worse prognosis (e.g. for C4d and MBL) |
| IC-MPGN | • Arises from deposition of immune complexes in the kidney, triggering the classical complement pathway • Dysregulation of the alternative complement pathway may underly pathogenesis of IC-MPGN o Around 50% of patients with IC-MPGN have genetic and/or acquired abnormalities that result in dysregulation of the alternative pathway o This includes genetic abnormalities in CFH, C3, CFI and CFB; and acquired factors such as C3 nephritic factors, or other autoantibodies against Factor H, Factor B and C3b |
| MN | • Characterised by glomerular deposition of immune complexes (most often involving IgG4) o MN can be due to autoantibodies (primary MN) or systemic disease (secondary MN) • Evidence suggests activation of the complement system contributes to MN o Dysfunction of complement regulatory proteins of the alternative pathway may contribute to pathogenesis o Complement deposition has been reported in the glomerulus (C3 [in 70–100% of patients], C5b9, C6, C4d); and C3 and IgG deposition has been reported in sub-epithelial immune complexes |
Evidence also suggests complement activation plays a key role in other kidney conditions such as lupus nephritis23. In lupus nephritis, altered clearance of immune complexes by complement is thought to result in immune complex deposition and complement activation23. This leads to glomerular inflammation, which may occur via C3a and C5-dependent inflammatory cell recruitment, and C5b-9-induced tissue damage23.
Overall, the role of complement in the pathophysiology of kidney diseases is complex, and will be further untangled with more research12. The strongest implication that a given complement pathway is involved in the pathogenesis of a kidney disease is provided by demonstrating a beneficial clinical effect from inhibiting specific complement components within that pathway12. Therefore, results from clinical trials of complement inhibitors across a range of kidney diseases are eagerly awaited4,5,11,13,46.
For clinicians, an improved knowledge of the role of complement activation in kidney disease may assist with selecting the optimal therapeutic target in the complement cascade, and may inform treatment selection in the future12.
Unmet needs in CMKDs
There are many unmet needs in the management of complement-mediated kidney diseases (CMKDs), particularly for improved diagnosis11,47 and new therapeutic approaches that target underlying disease pathophysiology11,48,49.
Current treatment options for CMKDs are limited, with frontline strategies to manage disease mainly consisting of corticosteroids and immunosuppressants50. Other treatment options include:
- Budesonide for IgA nephropathy (IgAN)51,52
- Eculizumab53,54 and ravulizumab55,56 for atypical hemolytic uremic syndrome (aHUS)
- Rituximab and calcineurin inhibitors (e.g. tacrolimus)50 for membranous nephropathy (MN)
No disease-specific treatment has been approved for C3 glomerulopathy (C3G)11, and no available treatments are designed to target the pathways underlying pathophysiology of the disease49. Furthermore, not all patients with aHUS achieve an adequate response to eculizumab5, and there is an increased risk of serious infections with use of eculizumab or ravulizumab5,12,53-56.
There is a need for new therapeutic approaches for CMKDs, particularly those that target key pathways involved in their underlying disease pathophysiology11,48,49
Several investigational treatments are currently in development for CMKDs, with the aim of improving outcomes and quality of life for patients4,5,12. In particular, complement inhibitors are a key area of interest for clinical development1,12,48, with potential to improve outcomes for patients with these devastating diseases12,48.
Complement inhibition – A promising treatment approach in CMKDs
The development of complement inhibitors represented one of the major breakthroughs in clinical nephrology in the last decade
Two complement inhibitors, eculizumab and ravulizumab, have received approval from the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for treatment of atypical hemolytic uremic syndrome (aHUS)53-56.
As we learn more about the complex pathophysiology of complement-mediated kidney diseases (CMKDs), more investigational treatments that target key drivers or mediators of these diseases are progressing through clinical development11,23,57.
The growing number of complement inhibitors in clinical development12 may help to address unmet needs for more effective treatment strategies for CMKDs11,48, with potential to improve outcomes for patients with these devastating diseases12,48
Join Dr Carla Nester as she describes some of the investigational treatments in clinical trials for C3G and IgAN.
Key therapeutic targets in the complement system are summarised in Figure 3, including approved medications and investigational drugs in development.
Figure 3. Therapeutic targets in the complement system for C3G, aHUS, IgAN and MN1,57 (Adapted1 under Creative Commons License CC BY 4.0). Complement inhibitors that are EMA- or FDA-approved for aHUS are indicated in green, and investigational drugs targeting the complement pathway are shown in blue. aHUS, atypical hemolytic uremic syndrome; C3G, C3 glomerulopathy; EMA, European Medicines Agency; FDA, US Food and Drug Administration; IgAN, IgA nephropathy; MASP2, mannose-binding lectin-associated serine protease 2; MN, membranous nephropathy.
Complement inhibitors approved for use in CMKDs
Eculizumab and ravulizumab are monoclonal antibodies that act on the terminal complement pathway, binding to complement protein C5 and preventing production of C5a and C5b-91,54,56. Their approved indications for aHUS are summarised in Table 3.
Table 3. Complement inhibitors with FDA and/or EMA approval for aHUS53,54. aHUS, atypical hemolytic uremic syndrome; EMA, European Medicines Agency; FDA, US Food and Drug Administration; TMA, thrombotic microangiopathy.
| Drug | FDA indication | EMA indication |
| Eculizumab | Treatment of patients with aHUS to inhibit complement-mediated TMA |
Treatment of adults and children with aHUS |
| Ravulizumab | Treatment of adult and paediatric patients one month of age and older with aHUS to inhibit complement-mediated TMA | Treatment of patients with a body weight of 10 kg or above with aHUS who are complement inhibitor treatment-naive or have received eculizumab for at least 3 months and have evidence of response to eculizumab |
The key clinical efficacy and safety data supporting these approvals were obtained from five single-arm studies for eculizumab (four phase 2 and one retrospective observational)53,54, and two open-label, single-arm phase 3 studies for ravulizumab55,56, across adult, adolescent and paediatric populations with aHUS53-56.
Since its approval for aHUS in 201158, eculizumab has emerged as part of standard of care and is considered to have transformed the prognosis of patients with the disease11,12. Engineered from eculizumab, ravulizumab is a longer acting inhibitor of C5, permitting an extended dosing interval of 2–8 weeks10.
Some complement inhibitors that are in development for CMKDs have received EMA or FDA approval for other conditions. These include:
- Avacopan, which is FDA-approved for anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis59, and EMA-approved for severe, active granulomatosis with polyangiitis (GPA or Wegener’s granulomatosis) or microscopic polyangiitis (MPA)60
- Pegcetacoplan, which is FDA-approved for paroxysmal nocturnal haemaglobinuria (PNH)61 and EMA-approved for patients with PNH and anaemia after treatment with a C5 inhibitor for ≥3 months62
Safety considerations for terminal pathway complement inhibitors
Patients receiving treatment with eculizumab or ravulizumab can be at increased risk of serious infections53-56, given these agents act as terminal pathway inhibitors2,5. The EMA and FDA prescribing information53-56 includes the following special warnings/precautions:
- Increased susceptibility to meningococcal infection (Neisseria meningitidis)53-56. To reduce this risk of infection, all patients must be vaccinated with meningococcal vaccines at least two weeks prior to initiating eculizumab or ravulizumab, unless the risk of delaying treatment therapy outweighs the risk of developing a meningococcal infection53-56
- Increased susceptibility to other serious infections, especially with Neisseria and encapsulated bacteria53-56. Caution is advised when administering these treatments to patients with active systemic infections53-56
Prior to commencing treatment with eculizumab or ravulizumab, it is recommended to initiate immunisations according to current immunisation guidelines53-56.
Investigational anti-complement therapies in CMKDs
Investigational therapies that target the complement cascade are in various stages of clinical development for CMKDs (Table 4).
Table 4. Investigational therapies in clinical development that target the complement system in kidney diseases57. aHUS, atypical hemolytic uremic syndrome; C3G, complement component 3 glomerulopathy; C3GN, C3 glomerulonephritis; DDD, dense deposit disease; IC-MPGN, immune complex membranoproliferative glomerulonephritis; IgAN, immunoglobulin A nephropathy; LN, lupus nephritis; MASP-2, mannose-binding lectin-associated serine protease-2; MN, membranous nephropathy; PNH, paroxysmal nocturnal haemoglobinuria. *Danicopan (a Factor D inhibitor) was previously investigated for C3G, IC-MPGN and DDD in clinical trials that have since been completed (NCT03124368, NCT03369236) or terminated (NCT03459443), and no longer appears to be under active development for CMKDs57. †Study has passed its completion date and status has not been verified in more than two years57. Note: This is intended as a summary and is not an exhaustive list of all complement inhibitors in clinical development. Information current as of 9 June 2023.
| Investigational therapy | Population/condition | Clinical trial phase (status) |
| C3 inhibitors | ||
| ARO-C3 | Healthy adults or volunteers with PNH or complement-mediated kidney disease (C3G or IgAN) | Phase 1/2a – NCT05083364 (recruiting) |
| Pegcetacoplan | IgAN, LN, MN, C3G (C3GN or DDD) | Phase 2 – NCT03453619 (active, not recruiting) |
| Post-transplant recurrence of C3G or IC-MPGN | Phase 2 – NCT04572854 (recruiting) | |
| C3G or IC-MPGN | Phase 3 – NCT05067127 (recruiting) | |
| C5a inhibitor | ||
| Avacopan | C3G | Phase 2 – NCT03301467 (completed) |
| aHUS | Phase 2 – NCT02464891 (terminated) | |
| IgAN | Phase 2 – NCT02384317 (completed) | |
| C5 inhibitors | ||
| Cemdisiran | IgAN | Phase 2 – NCT03841448 (active, not recruiting) |
| Crovalimab | aHUS | Phase 3 • Paediatric: NCT04958265 (recruiting) • Adolescents and adults: NCT04861259 (recruiting) |
| Ravulizumab | IgAN | Phase 2 – NCT04564339 (recruiting) |
| aHUS | Phase 3 • NCT03131219 (completed) • NCT02949128 (completed) |
|
| Bispecific anti-C3/C5 | ||
| KP104 | IgAN | Phase 2 – NCT05517980 (not yet recruiting) |
| Factor B inhibitor | ||
| Iptacopan | C3G | Phase 2 – NCT03832114 (completed) Phase 3 – NCT04817618 (recruiting) |
| IgAN | Phase 2 – NCT03373461 (completed) Phase 3 – NCT04578834 (recruiting) |
|
| aHUS | Phase 3 – NCT04889430 (recruiting) Phase 4 – NCT02574403 (completed) |
|
| MN | Phase 2 – NCT04154787 (terminated) | |
| IONIS-FB-LRx | IgAN | Phase 2 – NCT04014335 (recruiting) |
| Factor Bb inhibitor | ||
| NM8074 | C3G | Phase 1 – NCT05647811 (not yet recruiting) |
| aHUS | Phase 2 – NCT05684159 (not yet recruiting) | |
| Factor D inhibitor* | ||
| Vemircopan | IgAN | Phase 2 – NCT05097989 (recruiting) |
| MASP-2 inhibitor | ||
| Narsoplimab | IgAN, LN, MN, C3G | Phase 2 – NCT02682407 (status unknown†) |
| IgAN | Phase 3 – NCT03608033 (status unknown†) | |
For CMKDs and other diseases involving complement, key investigational therapeutic targets in the complement cascade include C3, Factor B, Factor D and mannose-binding lectin-associated serine protease-2 (MASP-2)57. Many of these investigational targets lie upstream of C5, the therapeutic target of eculizumab and ravulizumab, and have potential to exert impact over earlier aspects of complement cascade activation, including formation of C3 and C5 convertase, and/or the amplification phase4.
As investigational inhibitors of complement components progress through clinical trials, it is hoped that novel therapies will become available to provide a range of effective treatment options for patients with CMKDs and other complement-mediated diseases5.
Within the next 1–2 years, it is very likely that one or more of these drugs will be available to the practicing nephrologist
As more targeted treatments emerge for clinical use, there is also major interest in identifying biomarkers to predict which patients are more likely to receive benefit from treatment with complement-targeted therapies11. Further research in this area may enable a more precise approach to targeted treatment selection in the future11.
Overall, there are many exciting developments on the horizon, with great potential to improve the lives of patients with CMKDs5,11.
Learn about C3G and explore key aspects of diagnosis, risk prediction, treatment and unmet needs
References
- Poppelaars F, Thurman JM. Complement-mediated kidney diseases. Mol Immunol. 2020;128:175-187.
- Willows J, Brown M, Sheerin NS. The role of complement in kidney disease. Clin Med (Lond). 2020;20(2):156-160.
- Thurman JM. Complement and the kidney: An overview. Adv Chronic Kidney Dis. 2020;27(2):86-94.
- Heiderscheit AK, Hauer JJ, Smith RJH. C3 glomerulopathy: Understanding an ultra-rare complement-mediated renal disease. Am J Med Genet C Semin Med Genet. 2022;190(3):344-357.
- Ort M, Dingemanse J, van den Anker J, Kaufmann P. Treatment of rare inflammatory kidney diseases: Drugs targeting the terminal complement pathway. Front Immunol. 2020;11:599417.
- Cedzyński M, Thielens NM, Mollnes TE, Vorup-Jensen T, editors (2019). The role of complement in health and disease. Online: Frontiers Media SA. Available at: https://www.frontiersin.org/research-topics/6698/the-role-of-complement-in-health-and-disease#overview.
- Mitchell RN. Chapter II.2.3 - Innate and adaptive immunity: The immune response to foreign materials. In: Ratner BD, Hoffman AS, Schoen FJ, Lemons JE, editors. Biomaterials Science (Third Edition): Academic Press; 2013. p. 512-533.
- Remuzzie G. Role of complement in kidney disease: State of the art. KDIGO Controversies Conference on the Role of Complement in Kidney Disease. September 2022. Plenary Presentation.2022. Available at: https://kdigo.org/conferences/controversies-conference-on-complement-in-ckd/.
- Ricklin D, Hajishengallis G, Yang K, Lambris JD. Complement: a key system for immune surveillance and homeostasis. Nat Immunol. 2010;11(9):785-797.
- Kant S, Kronbichler A, Sharma P, Geetha D. Advances in understanding of pathogenesis and treatment of immune-mediated kidney disease: A review. Am J Kidney Dis. 2022;79(4):582-600.
- Meuleman MS, Grunenwald A, Chauvet S. Complement C3-targeted therapy in C3 glomerulopathy, a prototype of complement-mediated kidney diseases. Semin Immunol. 2022:101634.
- Fakhouri F, Schwotzer N, Golshayan D, Frémeaux-Bacchi V. The rational use of complement inhibitors in kidney diseases. Kidney International Reports. 2022.
- So BYF, Chan GCW, Yap DYH, Chan TM. The role of the complement system in primary membranous nephropathy: A narrative review in the era of new therapeutic targets. Front Immunol. 2022;13:1009864.
- Michels M, van de Kar N, van Kraaij SAW, Sarlea SA, Gracchi V, Engels F, et al. Different aspects of classical pathway overactivation in patients with C3 glomerulopathy and immune complex-mediated membranoproliferative glomerulonephritis. Front Immunol. 2021;12:715704.
- Goodship TH, Cook HT, Fakhouri F, Fervenza FC, Frémeaux-Bacchi V, Kavanagh D, et al. Atypical hemolytic uremic syndrome and C3 glomerulopathy: conclusions from a “Kidney Disease: Improving Global Outcomes”(KDIGO) Controversies Conference. Kidney Int. 2017;91(3):539-551.
- Nester CM, Barbour T, de Cordoba SR, Dragon-Durey MA, Fremeaux-Bacchi V, Goodship TH, et al. Atypical aHUS: State of the art. Mol Immunol. 2015;67(1):31-42.
- Yan K, Desai K, Gullapalli L, Druyts E, Balijepalli C. Epidemiology of atypical hemolytic uremic syndrome: A systematic literature review. Clin Epidemiol. 2020;12:295-305.
- Alok A, Yadav A. Membranous Nephropathy. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright 2022, StatPearls Publishing LLC; 2020.
- Sethi S, Fervenza FC. Membranoproliferative glomerulonephritis--a new look at an old entity. N Engl J Med. 2012;366(12):1119-1131.
- Daina E, Cortinovis M, Remuzzi G. Kidney diseases. Immunological Reviews. 2023;313(1):239-261.
- Haddad G, Lorenzen JM, Ma H, de Haan N, Seeger H, Zaghrini C, et al. Altered glycosylation of IgG4 promotes lectin complement pathway activation in anti-PLA2R1-associated membranous nephropathy. J Clin Invest. 2021;131(5).
- Le Stang MB, Gleeson PJ, Daha MR, Monteiro RC, van Kooten C. Is complement the main accomplice in IgA nephropathy? From initial observations to potential complement-targeted therapies. Mol Immunol. 2021;140:1-11.
- Fakhouri F, Schwotzer N, Golshayan D, Frémeaux-Bacchi V. The rational use of complement inhibitors in kidney diseases. Kidney Int Rep. 2022;7(6):1165-1178.
- Kościelska-Kasprzak K, Bartoszek D, Myszka M, Żabińska M, Klinger M. The complement cascade and renal disease. Arch Immunol Ther Exp. 2014;62(1):47-57.
- Wang X, Van Lookeren Campagne M, Katschke KJ, Jr., Gullipalli D, Miwa T, Ueda Y, et al. Prevention of fatal C3 glomerulopathy by recombinant complement receptor of the Ig superfamily. J Am Soc Nephrol. 2018;29(8):2053-2059.
- Glassock RJ. Mortality Risk in IgA Nephropathy. J Am Soc Nephrol. 2019;30(5):720-722.
- Barratt J, Feehally J. IgA Nephropathy. J Am Soc Nephrol. 2005;16(7):2088-2097.
- Rajasekaran A, Julian BA, Rizk DV. IgA Nephropathy: An Interesting Autoimmune Kidney Disease. Am J Med Sci. 2021;361(2):176-194.
- Schena FP, Esposito P, Rossini M. A narrative review on C3 glomerulopathy: A rare renal disease. Int J Mol Sci. 2020;21(2):525.
- Smith RJH, Appel GB, Blom AM, Cook HT, D'Agati VD, Fakhouri F, et al. C3 glomerulopathy - understanding a rare complement-driven renal disease. Nat Rev Nephrol. 2019;15(3):129-143.
- Smith RJ, Alexander J, Barlow PN, Botto M, Cassavant TL, Cook HT, et al. New approaches to the treatment of dense deposit disease. J Am Soc Nephrol. 2007;18(9):2447-2456.
- Storrar J, Chinnadurai R, Sinha S, Kalra PA. The epidemiology and evolution of IgA nephropathy over two decades: A single centre experience. PLoS One. 2022;17(9):e0268421.
- Lubbers R, van Essen MF, van Kooten C, Trouw LA. Production of complement components by cells of the immune system. Clin Exp Immunol. 2017;188(2):183-194.
- Zipfel PF, Skerka C. Complement regulators and inhibitory proteins. Nat Rev Immunol. 2009;9(10):729-740.
- Markiewski MM, Lambris JD. The role of complement in inflammatory diseases from behind the scenes into the spotlight. Am J Pathol. 2007;171(3):715-727.
- Mevorach D, Mascarenhas JO, Gershov D, Elkon KB. Complement-dependent clearance of apoptotic cells by human macrophages. J Exp Med. 1998;188(12):2313-2320.
- Barratt J, Weitz I. Complement Factor D as a Strategic Target for Regulating the Alternative Complement Pathway. Frontiers in Immunology. 2021;12.
- Gao S, Cui Z, Zhao MH. The Complement C3a and C3a Receptor Pathway in Kidney Diseases. Front Immunol. 2020;11:1875.
- Juul-Madsen HR, Viertlböeck B, Härtle S, Smith AL, Göbel TW. Chapter 7 - Innate immune responses. In: Schat KA, Kaspers B, Kaiser P, editors. Avian Immunology (Second Edition). Boston: Academic Press; 2014. p. 121-147.
- Piras R, Breno M, Valoti E, Alberti M, Iatropoulos P, Mele C, et al. CFH and CFHR copy number variations in C3 glomerulopathy and immune complex-mediated membranoproliferative glomerulonephritis. Front Genet. 2021;12:670727.
- Fremeaux-Bacchi V, Fakhouri F, Garnier A, Bienaimé F, Dragon-Durey M-A, Ngo S, et al. Genetics and outcome of atypical hemolytic uremic syndrome: A nationwide French series comparing children and adults. Clin J Am Soc Nephrol. 2013;8(4):554-562.
- Salant DJ. Targeting complement C5 in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 2011;22(1):7-9.
- Rizk DV, Maillard N, Julian BA, Knoppova B, Green TJ, Novak J, et al. The emerging role of complement proteins as a target for therapy of IgA nephropathy. Front Immunol. 2019;10:504.
- Medjeral-Thomas NR, Cook HT, Pickering MC. Complement activation in IgA nephropathy. Semin Immunopathol. 2021;43(5):679-690.
- Noris M, Daina E, Remuzzi G. Membranoproliferative glomerulonephritis: no longer the same disease and may need very different treatment. Nephrol Dial Transplant. 2021.
- Nester C. Glomerular diseases in which complement is emerging as a driver of injury: IgAN, MN, FSGS, diabetic nephropathy defined. Controversies Conference on the Role fo Complement in Kidney Disease. Florence, Italy; September 20222022. Available at: https://kdigo.org/conferences/controversies-conference-on-complement-in-ckd/.
- Feldman D, Bomback A, Nester C. National Kidney Foundation. The voice of the patient - C3 glomerulopathy (C3G). 2018. Available at: https://www.kidney.org/sites/default/files/C3G_EL-PFDD_VoP-Report_3-29-18.pdf.
- Andrighetto S, Leventhal J, Zaza G, Cravedi P. Complement and Complement Targeting Therapies in Glomerular Diseases. Int J Mol Sci. 2019;20(24).
- Martín B, Smith RJH. C3 Glomerulopathy. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, et al., editors. GeneReviews(®). Seattle (WA): University of Washington, Seattle
Copyright © 1993-2023, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved.; 1993. - Kidney Disease: Improving Global Outcomes Diabetes Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Oct 2021.
- Kinpeygo summary of product characteristics. 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/kinpeygo-epar-product-information_en.pdf. Accessed 31 January 2023.
- Calliditas Therapeutics AB. Budesonide (Tarpeyo) Full Prescribing Information (US FDA). US Food and Drug AdministrationDecember 2021. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215935s000lbl.pdf. Accessed 31 January 2023.
- Soliris summary of product characteristics. 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/soliris-epar-product-information_en.pdf. Accessed 31 January 2023.
- Soliris prescribing information. 2020. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/125166s434lbl.pdf. Accessed 31 January 2023.
- Ultomiris summary of product characteristics. 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/ultomiris-epar-product-information_en.pdf. Accessed 31 January 2023.
- Ultomiris (ravulizumab-cwvz) prescribing information. 2022. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/761108s021lbl.pdf. Accessed 31 January 2023.
- National Institutes of Health US National Library of Medicine. Clinicaltrials.gov. https://clinicaltrials.gov/ct2/home. Accessed 12 January 2023.
- Alexion Pharmaceuticals Inc,, 2014. FDA approves conversion of Soliris (eculizumab) accelerated approval in aHUS to regular approval for the treatment of patients with aHUS [press release]. Available at: https://media.alexion.com/news-releases/news-release-details/fda-approves-conversion-solirisr-eculizumab-accelerated-approval. Accessed 25 November 2022.
- US Food and Drug Administration, October 2021. FDA approves add-on drug for adults with rare form of blood vessel inflammation [press release]. Available at: https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-add-drug-adults-rare-form-blood-vessel-inflammation. Accessed 31 January 2023.
- Tavneos summary of product characteristics. 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/tavneos-epar-product-information_en.pdf. Accessed 31 January 2023.
- US Food and Drug Administration, May 2021. FDA approves new treatment for adults with serious rare blood disease [press release]. Available at: https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-new-treatment-adults-serious-rare-blood-disease. Accessed 31 January 2023.
- Aspaveli summary of product characteristics. 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/aspaveli-epar-product-information_en.pdf. Accessed 31 January 2023.
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.

