C3 glomerulopathy (C3G)
What is C3 glomerulopathy?
About C3 glomerulopathy
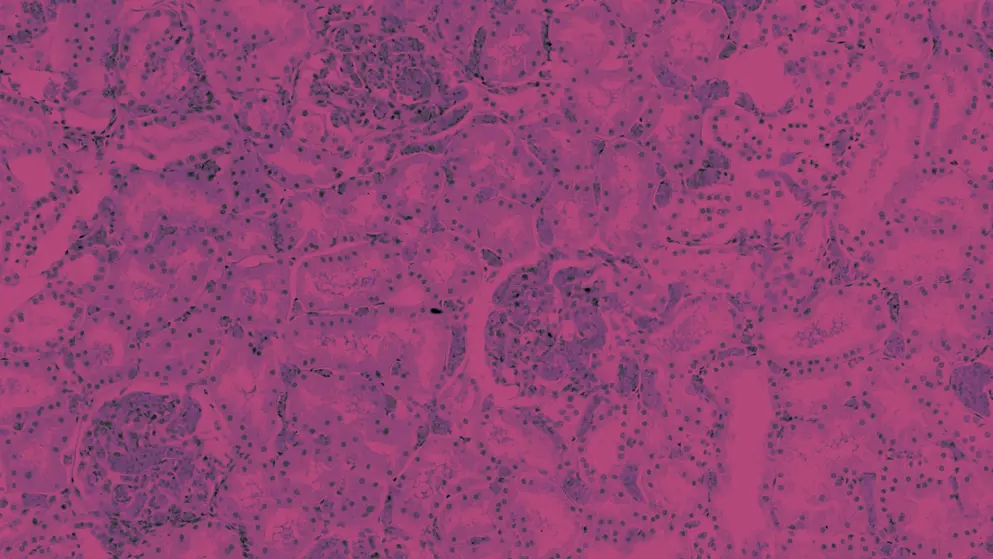
C3 glomerulopathy (C3G) is a rare and complex kidney disease that is primarily driven by dysregulation and excessive activation of the alternative complement pathway1,2
C3G is characterised by dominant deposition of the complement component C3 in the renal glomeruli2,3, resulting in chronic and irreversible kidney damage over time4 (Figure 1).
Figure 1. Complement system dysregulation in the pathophysiology of C3 glomerulopathy1,3-8. C3, complement component 3; C5, complement component 5; C3G, C3 glomerulopathy; GBM, glomerular basement membrane.
C3G is rare, with a prevalence of around 0.2–5 cases per million in the US and Europe4,9. It is most often diagnosed during childhood or young adulthood, and the median age at diagnosis is 22 years1.
Treatment options for C3G are currently limited, and renal prognosis remains poor without disease-specific treatment options1. Approximately 30–50% of patients with C3G progress to kidney failure within 10 years of diagnosis3. Almost all patients who undergo kidney transplantation experience disease recurrence, leading to renal allograft loss in up to 50% of patients within 10 years10.
Gain key insights from nephrologist Dr Carla Nester as she gives a brief overview of the current research being conducted into the causes of complement-mediated kidney diseases (CMKDs), including C3G and IgA nephropathy (IgAN).
Signs and symptoms of C3 glomerulopathy
C3G is a heterogeneous disease with variable clinical presentation4. Approximately one-third of adults with C3G present with acute kidney failure3.
The most common signs and symptoms of C3G are haematuria, proteinuria and nephrotic syndrome3. Others include:
- Signs of glomerulonephritis, often including hypertension3,11
- Impaired kidney function3 and/or signs of acute and chronic kidney injury11
- Low serum levels of C3 (most patients)3,5
- Reduced estimated glomerular filtration3
Extrarenal manifestations in people with C3G may include premature onset of retinal drusen12,13 and, rarely, acquired partial lipodystrophy12,14.
Role of complement dysregulation in the pathophysiology of C3 glomerulopathy
Excessive activation of the alternative complement pathway15 is observed in the majority (>90%) of patients with C3G4 and is considered causal1,5,15
For the remaining <10% of patients with C3G, complement dysregulation occurs in the classical and/or lectin pathways4.
The central pathological mechanism of C3G is C3 convertase overactivation1, and dysregulation of the C5/C5 convertase axis has been implicated in disease severity and phenotype1.
As a result of this complement dysregulation, continuous local complement activity leads to C3 deposition in the glomerulus, particularly C3b deposits in the glycocalyx4,5. Complement deposition in the glomerulus has been associated with4,6,16:
- activation and proliferation of endothelial and mesangial cells
- migration of immune cells to the glomerular compartment
- thickening of the glomerular basement membrane (GBM)
- podocyte dysfunction
- mesangial cell injury
This deposition can disrupt membrane function and trigger an inflammatory response, leading to glomerular damage5. Over time, inflammation and scarring can result in chronic and irreversible kidney damage4.
Causes of complement dysregulation in C3 glomerulopathy
Drivers of complement dysregulation in C3G can be acquired or genetic (Table 1)4.
Table 1. Acquired and genetic causes of complement dysregulation in C3 glomerulopathy3,4,7,8. C3GN, C3 glomerulonephritis; C3Nefs, complement component 3 nephritic factor; C4Nefs, complement component 4 nephritic factors; C5Nefs, complement component 5 nephritic factors; CFHR1–CFHR5, complement factor H-related 1–5; DDD, dense deposit disease. *A specific gene-variant subtype of C3GN, CFHR5 nephropathy, is endemic to Cyprus (where it affects ~1 in 6,000 persons)3.
| Causes of C3G | Factors contributing to complement dysregulation in C3G |
| Acquired | • C3Nefs: C3Nefs against the C3 convertase of the alternative pathway (C3bBb) are most common (reported in 50–80% of DDD and 44–50% of C3GN) • C4Nefs: Less frequent in C3G • C5Nefs: Common in C3G, associated with C3GN Other autoantibodies: • Anti-Factor H • Anti-Factor B • Anti-C3b Paraproteins (monoclonal immunoglobulins) |
| Genetic | Rare, disease-associated variants or genomic rearrangements in complement genes observed in ~25% of patients with C3G Genetic variants associated with susceptibility in C3G (potentially causal): • C3 convertase genes: C3, CFB • Complement regulatory genes: CFH, CFI • CFHR1–CHRF5 genes* |
The most commonly detected drivers of complement dysregulation in C3G are autoantibodies to the C3 and C5 convertases, which disrupt regulation of normal convertase or protein function3,4. Nephritic factors are autoantibodies commonly found in C3G that act to stabilise C3 or C5 convertases and prolong their half-life, leading to C3 or C5 consumption, respectively (Figure 2)3,4.
Figure 2. Mechanism of action of nephritic factors on regulation of the complement pathway (Adapted17 under Creative Commons Attribution License (CC BY 4.0). Nephritic factors are autoantibodies commonly found in C3G3 that stabilise and prolong the half-life of C3 and/or C5 convertases3,7,11, leading to chronic and unregulated complement activation in the fluid phase11. (A) C3Nef binds to C3 convertase in the alternative pathway, which prevents its spontaneous Factor H-mediated decay17. (B) C5Nef binds to C5 convertase of the alternative pathway in the presence of properdin (P), which prevents its spontaneous and regulator-mediated decay17. (C/D) C4Nef binds to C3/C5 convertases in the classical/lectin pathway, which prevents their spontaneous, regulator-mediated decay17. Soluble and membrane regulators of the complement system are indicated in red boxes. CR1, complement receptor 1; C3Nef, C3 nephritic factors; C4BP, C4 binding protein; C4Nef, C4 nephritic factors; C5Nef, C5 nephritic factors; DAF, decay accelerating factor; FH, Factor H; FI, Factor I; MCP, membrane cofactor protein.
Diagnosing C3 glomerulopathy
Overview of differential diagnosis for C3 glomerulopathy
Diagnosing C3 glomerulopathy (C3G) requires analysis of kidney biopsy tissue using light microscopy, immunofluorescence and electron microscopy2. However, C3G is heterogenous in presentation and outcomes18, and its clinical presentation overlaps with a number of other glomerulopathies and C3-dominant kidney diseases2,3.
Hear from Dr Carla Nester as she explains some of the key points to consider during differential diagnosis of C3G and related diseases.
For an overview of the steps involved in the differential diagnosis of C3G in practice, view our infographic below.
Overlap between C3 glomerulopathy and other conditions
Given the overlap in their clinical presentation and characteristics, differential diagnosis is required to distinguish between C3G and2:
- Immune complex-mediated membranoproliferative glomerulonephritis (IC-MPGN, also known as immune complex glomerulonephritis19), including monoclonal gammopathy
- Post-infectious glomerulonephritis (PIGN)
- C4 glomerulopathy (C4G)
- Other conditions that result in an MPGN pattern of kidney injury, such as antiphospholipid syndrome and thrombotic microangiopathy
Initial workup based on clinical presentation
For patients presenting with signs and symptoms of C3G, initial workup and considerations for kidney biopsy are summarised in Table 23.
Table 2. Initial workup based on clinical presentation and considerations for kidney biopsy2,3.
| Signs and symptoms | Investigation |
| If any of the following are present: • Proteinuria • Haematuria (macroscopic or microscopic) • Hypertension • Signs and symptoms of kidney function impairment (renal insufficiency, nephrotic syndrome, and/or nephritic syndrome) |
The following investigations should be undertaken: • Complete blood count • C3, C4 • Antinuclear antibodies • Antineutrophil cytoplasmic antibodies • Urine protein:creatinine ratio • Screening for hepatitis and other infections (if indicated) |
| If persistent proteinuria, a reduced glomerular filtration rate and/or unexplained hypertension If glomerulonephritis symptoms persist and C3 remains abnormal for ≥12 weeks |
Consider kidney biopsy |
| Proteinuria and/or glomerular haematuria | Kidney biopsy should be performed if: • the result is expected to modify treatment • and/or if additional prognostic information is needed |
Differential diagnosis based on kidney biopsy analysis
MPGN is the most commonly found lesion in C3G20. For patients with this pattern of kidney injury, the following practice points from the 2021 KDIGO guidelines inform differential diagnosis2,3.
A diagnosis of C3G is based on immunofluorescence analysis of a kidney biopsy specimen, which must demonstrate a dominant C3 deposition in the renal glomerulus (≥2 orders of magnitude greater than any other immune reactant)2.
Before assigning a C3G diagnosis, other C3-dominant glomerular lesions should be excluded2,3. These include PIGN and, for patients aged >50 years, monoclonal gammopathy 2,3.
Once a diagnosis of C3G is confirmed, electron microscopy is used to determine the disease subgroup2,3:
- Dense deposit disease (DDD) – defined by the presence of highly electron-dense, osmophilic, predominantly intramembranous deposits2
- C3 glomerulonephritis (C3GN) – involves mesangial and capillary wall deposits of lesser intensity2
Evaluations for complement dysregulation
Evaluations for complement dysregulation may be undertaken to inform treatment planning for patients with C3G (Table 3)3. However, the 2021 KDIGO guidelines only recommend evaluations for complement dysregulation in cases of IC-MPGN where no underlying aetiology has been found after extensive workup2.
Table 3. Evaluations for complement dysregulation2,3. AP50, complement alternate pathway activation 50%; Bb, cleavage product of factor B; C3Nefs, complement component 3 nephritic factors; C4Nefs, complement component 4 nephritic factors; C5Nefs, complement component 5 nephritic factors; CFHR5, complement factor H-related 5; CH50, complement haemolytic activity 50%; DGKE, diacylglycerol kinase epsilon; FB, factor B; FBAA, factor B autoantibodies; FH, factor H; FHAA, factor H autoantibodies; FI, factor I; Ig, immunoglobulin; IgA, immunoglobulin A; IgG, immunoglobulin G; IgM, immunoglobulin M; MLPA, multiplex-ligation-dependent probe amplification; sMAC, soluble membrane attack complex. *Recommended in Heiderscheit et al 20223, but not included in recommended evaluations for complement dysregulation in 2021 KDIGO Guidelines2.
| Evaluation | Components evaluated |
| Evaluations for complement dysregulation | Functional assays: CH50, AP50, Factor H function Complement components and regulators: C3, C4, Factor I, Factor H, Factor B, Properdin; plus C3b, C3c, C5bb* Measurement of complement activation: C3d, Bb, sMAC |
| Evaluations for possible drivers of complement dysregulation | Autoantibodies: anti-FH, anti-Factor B, nephritic factors (C3, C4, C5) Genetic testing: genetic variants in C3, CFH, CFI, CFB, CFHR1-5 MLPA; and DGKE* |
| Investigations for plasma cell disorders | Serum free light chains, serum and urine electrophoresis, and immunofixation |
| Immunofluorescence studies on kidney biopsy specimens | IgA, IgG, IgM, C1q, C3, fibrinogen, kappa and lambda light chains, C4d |
Some complement assays may require referral to specialist/research laboratories, and interpretation of complement assays may require expert consultation2.
Determining the degree and cause of dysregulation in the complement pathways may facilitate development of tailored treatment plans3
Although no complement inhibitors have been approved for use in patients with C3G21,22, numerous investigational candidates that target the complement system are in clinical development for C3G and other types of complement-mediated kidney diseases (CMKDs)23.
Challenges with C3 glomerulopathy diagnosis in practice
Aspects that can confound or complicate C3G diagnosis include3,24,25:
- Borderline immunofluorescence results2,16 (e.g. for C3G versus IC-MPGN)
- Biopsies changing from IC-MPGN to C3G over time3 (or vice versa16)
The boundary between C3G and IC-MPGN can be unclear, and dysregulation of the alternative complement pathway has been identified in some patients with IC-MPGN20.
In some cases, C3G may be triggered by infectious diseases, which can present a challenge for differentiating C3G diagnosis from PIGN1.
Additionally, not all antibodies used for routine immunofluorescence studies detect deposition of the predominant C3 cleavage product (C3dg), so complement fragment deposition may be missed24.
Risk prediction in C3 glomerulopathy
As C3 glomerulopathy (C3G) is a progressive disease with heterogenous outcomes18,20,27, individual patient outcomes are hard to predict28. In recent years, there has been interest in developing approaches and tools to predict prognosis in C3G28-31.
Join Dr Edwin Wong as he discusses several key causes of poor prognosis and useful endpoints in clinical trials for the treatment of C3G.
Predicting prognosis from C3 glomerulopathy diagnosis
Some clinical and histological parameters at diagnosis may predict outcomes for patients with C3G20.
- In cohort studies, kidney survival (i.e. the absence of kidney failure) has been predicted using clinical parameters such as age16 and estimated glomerular filtration rate (eGFR)29 at diagnosis, and serum creatinine levels and degree of proteinuria at clinical presentation32
- Histologic predictors of disease outcomes vary across studies, but generally include measurements of disease activity and disease chronicity on kidney biopsy16,20,27,29
A summary of investigational approaches to predict prognosis of C3G is shown in Table 4.
Table 4. Emerging and investigational approaches to predict prognosis of patients with C3G at diagnosis28-31. eGFR, estimated glomerular filtration rate; C3G, C3 glomerulopathy. *Activity score included mesangial hypercellularity, endocapillary proliferation, membranoproliferative morphology, leukocyte infiltration, crescent formation, fibrinoid necrosis and interstitial inflammation in kidney biopsy29. †Chronicity score included glomerulosclerosis, tubular atrophy, interstitial fibrosis and arteriosclerosis30. ‡Total chronicity score was calculated from Columbia University’s C3G Histologic Index (C3G-HI) 28.
| Approach | Characteristics/factors evaluated in model | Risk prediction |
| C3G Histologic Index (C3G-HI) score | • Activity score* • Chronicity score† The total activity and total chronicity scores were the strongest predictors of progression |
To predict risk of progression to kidney failure in patients with C3G |
| Histologic scoring index (total chronicity score) | Total chronicity score, based on: • C3G-HI activity* • chronicity score† |
To predict risk of progression to kidney failure in patients with C3G |
| Nomogram | Baseline: • eGFR • proteinuria • total chronicity score in kidney biopsy‡ |
To predict risk of progression to kidney failure in C3G patients at 1,2,5 and 10 years, using data at baseline (diagnosis) |
| Three-point C3G prognostic score | • Profile of biomarkers of C3 and C5 convertases (C3 and/or sC5b-9) • eGFR at presentation • Rare disease-predicting variants in complement genes |
• To predict risk of worse prognosis/ progression to kidney failure • May help stratify adult patients into subgroups that require close monitoring and more aggressive therapy |
Other histologic parameters identified as determinants of kidney failure in C3G include interstitial fibrosis/tubular atrophy, cellular/fibrocellular crescent and segmental sclerosis18.
Tools to predict prognosis in C3G may inform management by helping to identify patients at greater risk of poor outcomes, who may therefore require close monitoring and more aggressive therapy31
Dynamic monitoring for C3 glomerulopathy prognosis over time
Increased levels of proteinuria over time have been associated with an increased risk of kidney failure in patients with C3G33. Pending further validation and research, proteinuria changes may become useful for dynamic prediction of kidney outcomes over time28,33.
Treating C3 glomerulopathy
Current treatment strategies for C3 glomerulopathy (C3G) are largely limited to symptomatic treatments2,3. These include:
- angiotensin converting enzyme (ACE) inhibitors/angiotensin receptor blockers (ARBs) to reduce proteinuria and improve blood pressure control2
- immunosuppressants such as mycophenolate mofetil (MMF) and glucocorticoids for moderate-to-severe disease2, to suppress kidney inflammation3
C3G treatments are summarised in Figure 3.
Figure 3. Recommended treatments for C3 glomerulopathy2. ACEi, angiotensin-converting enzyme inhibitor; ARBs, angiotensin receptor blockers; C3G, C3 glomerulopathy; CV, cardiovascular; MMF, mycophenolate mofetil. *Defined as moderate-to-marked proliferation on biopsy and proteinuria (>2 g/d)2. †For hypertension/proteinuria, other strategies include mineralocorticoid receptor antagonists, loop and thiazide diuretics2.‡Notes: Although eculizumab may be considered in this population, there is no clear evidence of benefit from eculizumab treatment in patients with C3G2, eculizumab is not FDA- or EMA-approved for use in patients with C3G (so use for this indication is considered off-label)21,34. §For hyperlipidaemia, other options include bile acid sequestrants, fibrates, nicotinic acid, ezetimibe, PCSK9 inhibitor, lipid apheresis2.
Guidelines note eculizumab may be considered for patients with moderate-to-severe C3G, if no response is achieved with MMF plus glucocorticoids2. However, eculizumab is not currently approved by the European Medicines Agency (EMA) or the US Food and Drug Administration (FDA) for use in patients with C3G35,36, and such use is considered off-label3. A few studies have indicated limited benefit from eculizumab in C3G, with more than 50% of patients non-responsive after >1 year of eculizumab treatment37,38.
No disease-specific treatments have been approved for C3G1,21,22; however, various investigational drugs that target the complement system are in clinical development for this indication39.
Addressing unmet needs in C3G treatment
Below, Dr Edwin Wong describes some of the most significant obstacles and unmet needs for management of C3 glomerulopathy (C3G).
Unmet needs in C3G management
In C3G, there are pressing needs for:
- improved and earlier diagnosis of C3G1,40,41
- effective treatment strategies that target underlying disease drivers1,3,42,43
Despite the use of supportive and immunosuppressive treatments30, the poor outcomes observed in patients with C3G today are similar to outcome data described more than 50 years ago41. Patients with C3G are at high risk of kidney failure30,44. Even after kidney transplant, there is a high risk of disease recurrence44. This persistently poor prognosis is considered to reflect the lack of effective, targeted treatment options for C3G1,3,43.
In a recent multicentre retrospective cohort study of patients with C3G, 43% of patients with C3G reached kidney failure after only 5 years, despite 84% receiving immunosuppression30
There is also a need for a better understanding of the natural history of C3G1, and many knowledge gaps persist3,4. An improved understanding of the natural history of C3G may:
- enable integration of clinical data with findings from pathology, genetic and complement biomarker studies4
- help to inform duration of treatment1
- clarify generalisability and relevance of natural history data to ethnically diverse populations29
- help to clarify if changes in dysregulated pathways may occur or normalise over time1
Investigational treatments in clinical development for C3G
To address the lack of targeted treatments for C3G1,43 a range of investigational treatments are in clinical development23,39. Key therapeutic targets within the complement cascade that are being investigated in clinical trials for C3G are summarised below23 (Table 5).
Table 5. Complement inhibitors in clinical trials for C3G23*. aHUS, atypical hemolytic uremic syndrome; C3G, complement component 3 glomerulopathy; C3GN, C3 glomerulonephritis; DDD, dense deposit disease; FB, factor B; FH, factor H; IC-MPGN, immune complex membranoproliferative glomerulonephritis; IgAN, immunoglobulin A nephropathy; LN, lupus nephritis; MASP-2, mannose-binding lectin-associated serine protease-2; MN, membranous nephropathy; PNH, paroxysmal nocturnal haemoglobinuria. *Danicopan (a Factor D inhibitor) was previously investigated for C3G, IC-MPGN and DDD in clinical trials that have since been completed (NCT03124368, NCT03369236) or terminated (NCT03459443), and no longer appears to be under active development for CMKDs23. †Study has passed its completion date and status has not been verified in more than two years23. Note: This is intended as a summary and is not an exhaustive list of all complement inhibitors in clinical development. Information current as of 9 June 2023.
| Investigational therapy | Population/condition | Clinical trial phase (status) |
| C3 inhibitors | ||
| ARO-C3 | Healthy adults or volunteers with PNH or complement-mediated renal disease (C3G or IgAN) | Phase 1/2a – NCT05083364 (recruiting) |
| Pegcetacoplan | IgAN, LN, MN, C3G (C3GN, DDD) | Phase 2 – NCT03453619 (active, not recruiting) |
| Post-transplant recurrence of C3G or IC-MPGN | Phase 2 – NCT04572854 (recruiting) | |
| C3G or IC-MPGN | Phase 3 – NCT05067127 (recruiting) | |
| C5a inhibitor | ||
| Avacopan | C3G | Phase 2 – NCT03301467 (completed) |
| Factor B inhibitor | ||
| Iptacopan | C3G | Phase 2 – NCT03832114 (completed) Phase 3 – NCT04817618 (recruiting) |
| Factor Bb inhibitor | ||
| NM8074 | C3G | Phase 1 – NCT05647811 (not yet recruiting) |
| MASP-2 inhibitor | ||
| Narsoplimab | IgAN, LN, MN, C3G | Phase 2 – NCT02682407 (status unknown†) |
As C3 convertase overactivation appears central to the pathophysiology of C3G, investigational treatments that target the C3/C3 convertase axis by inhibiting C3, Factor B or Factor D are emerging as promising therapeutic approaches for C3G1.
Find out more about types of CMKDs, and learn about their burden and impact
Learn about the complement system and how it becomes dysregulated in disease
Learn about the burden and pathophysiology of IgA nephropathy, another type of CMKD
Test your knowledge on C3 glomerulopathy
Challenge your knowledge by answering four questions in this short quiz on C3 glomerulopathy (C3G). Your answers will also help to improve the quality of medical education on Medthority.
Meet Tamara
Tamara, 22 years of age, has presented to your clinic with symptoms of fatigue and discoloured (light pink), foamy urine, which she has had for the past 3 months. She has also been experiencing frequent infections over the past year.
Based on your initial investigations (including blood pressure, urinalysis and blood test results), you suspect C3G as one of the differential diagnoses, and refer Tamara for a kidney biopsy.
References
- Meuleman MS, Grunenwald A, Chauvet S. Complement C3-targeted therapy in C3 glomerulopathy, a prototype of complement-mediated kidney diseases. Semin Immunol. 2022:101634.
- Kidney Disease: Improving Global Outcomes Diabetes Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Oct 2021.
- Heiderscheit AK, Hauer JJ, Smith RJH. C3 glomerulopathy: Understanding an ultra-rare complement-mediated renal disease. Am J Med Genet C Semin Med Genet. 2022;190(3):344-357.
- Smith RJH, Appel GB, Blom AM, Cook HT, D'Agati VD, Fakhouri F, et al. C3 glomerulopathy - understanding a rare complement-driven renal disease. Nat Rev Nephrol. 2019;15(3):129-143.
- Willows J, Brown M, Sheerin NS. The role of complement in kidney disease. Clin Med (Lond). 2020;20(2):156-160.
- Zipfel PF, Wiech T, Stea ED, Skerka C. CFHR Gene Variations Provide Insights in the Pathogenesis of the Kidney Diseases Atypical Hemolytic Uremic Syndrome and C3 Glomerulopathy. J Am Soc Nephrol. 2020;31(2):241-256.
- Kant S, Kronbichler A, Sharma P, Geetha D. Advances in understanding of pathogenesis and treatment of immune-mediated kidney disease: A review. Am J Kidney Dis. 2022;79(4):582-600.
- Servais A, Noel L-H, Roumenina LT, Le Quintrec M, Ngo S, Dragon-Durey M-A, et al. Acquired and genetic complement abnormalities play a critical role in dense deposit disease and other C3 glomerulopathies. Kidney Int. 2012;82(4):454-464.
- Schena FP, Esposito P, Rossini M. A narrative review on C3 glomerulopathy: A rare renal disease. Int J Mol Sci. 2020;21(2):525.
- Ahmad SB, Bomback AS. C3 glomerulopathy: pathogenesis and treatment. Adv Chronic Kidney Dis. 2020;27(2):104-110.
- Ort M, Dingemanse J, van den Anker J, Kaufmann P. Treatment of rare inflammatory kidney diseases: Drugs targeting the terminal complement pathway. Front Immunol. 2020;11:599417.
- Goodship TH, Cook HT, Fakhouri F, Fervenza FC, Frémeaux-Bacchi V, Kavanagh D, et al. Atypical hemolytic uremic syndrome and C3 glomerulopathy: conclusions from a “Kidney Disease: Improving Global Outcomes”(KDIGO) Controversies Conference. Kidney Int. 2017;91(3):539-551.
- Savige J, Amos L, Ierino F, Mack HG, Symons RCA, Hughes P, et al. Retinal disease in the C3 glomerulopathies and the risk of impaired vision. Ophthalmic Genet. 2016;37(4):369-376.
- Corvillo F, López-Trascasa M. Acquired partial lipodystrophy and C3 glomerulopathy: Dysregulation of the complement system as a common mechanism. Nefrología (English Edition). 2018;38(3):258-266.
- Kaartinen K, Safa A, Kotha S, Ratti G, Meri S. Complement dysregulation in glomerulonephritis. Semin Immunol. 2019;45:101331.
- Caravaca-Fontán F, Lucientes L, Cavero T, Praga M. Update on C3 glomerulopathy: a complement-mediated disease. Nephron. 2020;144(6):272-280.
- Corvillo F, Okrój M, Nozal P, Melgosa M, Sánchez-Corral P, López-Trascasa M. Nephritic factors: an overview of classification, diagnostic tools and clinical associations. Front Immunol. 2019;10:886.
- Lomax-Browne HJ, Medjeral-Thomas NR, Barbour SJ, Gisby J, Han H, Bomback AS, et al. Association of histologic parameters with outcome in C3 glomerulopathy and idiopathic immunoglobulin-associated membranoproliferative glomerulonephritis. Clin J Am Soc Nephrol. 2022;17(7):994-1007.
- Daina E, Cortinovis M, Remuzzi G. Kidney diseases. Immunological Reviews. 2023;313(1):239-261.
- Caravaca-Fontán F, Praga M. Prognostication for C3 Glomerulopathy and Idiopathic Immunoglobulin-Associated Membranoproliferative Glomerulonephritis. Clin J Am Soc Nephrol. 2022;17(7):945-948.
- European Medicines Agency. Medicines. https://www.ema.europa.eu/en/medicines?search_api_views_fulltext=c3+glomerulopathy. Accessed 12 January 2023.
- US Food and Drug Administration. Drugs@FDA: FDA-approved drugs. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm. Accessed 05 December 2022.
- National Institutes of Health US National Library of Medicine. Clinicaltrials.gov. https://clinicaltrials.gov/ct2/home. Accessed 12 January 2023.
- Sethi S, Vrana JA, Fervenza FC, Theis JD, Sethi A, Kurtin PJ, et al. Characterization of C3 in C3 glomerulopathy. Nephrol Dial Transplant. 2017;32(3):459-465.
- Iatropoulos P, Noris M, Mele C, Piras R, Valoti E, Bresin E, et al. Complement gene variants determine the risk of immunoglobulin-associated MPGN and C3 glomerulopathy and predict long-term renal outcome. Mol Immunol. 2016;71:131-142.
- Iatropoulos P, Daina E, Curreri M, Piras R, Valoti E, Mele C, et al. Cluster analysis identifies distinct pathogenetic patterns in C3 glomerulopathies/immune complex-mediated membranoproliferative GN. J Am Soc Nephrol. 2018;29(1):283-294.
- Ravindran A, Fervenza FC, Smith RJ, De Vriese AS, Sethi S. C3 glomerulopathy: ten years' experience at Mayo Clinic. Presented at the Mayo Clinic Proceedings 2018.
- Caravaca-Fontán F, Rivero M, Cavero T, Díaz-Encarnación M, Cabello V, Ariceta G, et al. Development and validation of a nomogram to predict kidney survival at baseline in patients with C3 glomerulopathy. Clin Kidney J. 2022;15(9):1737-1746.
- Bomback AS, Santoriello D, Avasare RS, Regunathan-Shenk R, Canetta PA, Ahn W, et al. C3 glomerulonephritis and dense deposit disease share a similar disease course in a large United States cohort of patients with C3 glomerulopathy. Kidney Int. 2018;93(4):977-985.
- Caravaca-Fontán F, Trujillo H, Alonso M, Díaz-Encarnación M, Cabello V, Ariceta G, et al. Validation of a Histologic Scoring Index for C3 Glomerulopathy. Am J Kidney Dis. 2021;77(5):684-695.e681.
- Chauvet S, Hauer JJ, Petitprez F, Rabant M, Martins PV, Baudouin V, et al. Results from a nationwide retrospective cohort measure the impact of C3 and soluble C5b-9 levels on kidney outcomes in C3 glomerulopathy. Kidney Int. 2022;102(4):904-916.
- Caravaca-Fontán F, Díaz-Encarnación MM, Lucientes L, Cavero T, Cabello V, Ariceta G, et al. Mycophenolate Mofetil in C3 Glomerulopathy and Pathogenic Drivers of the Disease. Clin J Am Soc Nephrol. 2020;15(9):1287-1298.
- Caravaca-Fontán F, Díaz-Encarnación M, Cabello V, Ariceta G, Quintana LF, Marco H, et al. Longitudinal change in proteinuria and kidney outcomes in C3 glomerulopathy. Nephrol Dial Transplant. 2022;37(7):1270-1280.
- US Food and Drug Administration. Drugs@FDA: FDA-approved drugs. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm. Accessed 12 January 2023.
- Soliris summary of product characteristics. 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/soliris-epar-product-information_en.pdf. Accessed 31 January 2023.
- Soliris prescribing information. 2020. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/125166s434lbl.pdf. Accessed 31 January 2023.
- Le Quintrec M, Lapeyraque A-L, Lionet A, Sellier-Leclerc A-L, Delmas Y, Baudouin V, et al. Patterns of clinical response to eculizumab in patients with C3 glomerulopathy. Am J of Kidney Dis. 2018;72(1):84-92.
- Bomback AS, Smith RJ, Barile GR, Zhang Y, Heher EC, Herlitz L, et al. Eculizumab for dense deposit disease and C3 glomerulonephritis. Clin J Am Soc Nephrol. 2012;7(5):748-756.
- Fakhouri F, Schwotzer N, Golshayan D, Frémeaux-Bacchi V. The rational use of complement inhibitors in kidney diseases. Kidney Int Rep. 2022;7(6):1165-1178.
- Feldman D, Bomback A, Nester C. National Kidney Foundation. The voice of the patient - C3 glomerulopathy (C3G). 2018. Available at: https://www.kidney.org/sites/default/files/C3G_EL-PFDD_VoP-Report_3-29-18.pdf.
- Cattran DC, Sethi S. Slowly Unraveling the Mysteries of C3G. Am J Kidney Dis. 2021;77(5):670-672.
- Andrighetto S, Leventhal J, Zaza G, Cravedi P. Complement and Complement Targeting Therapies in Glomerular Diseases. Int J Mol Sci. 2019;20(24).
- Michels MAHM, Wijnsma KL, Kurvers RAJ, Westra D, Schreuder MF, van Wijk JAE, et al. Long-term follow-up including extensive complement analysis of a pediatric C3 glomerulopathy cohort. Pediatric Nephrology. 2022;37(3):601-612.
- Fakhouri F, Le Quintrec M, Frémeaux-Bacchi V. Practical management of C3 glomerulopathy and Ig-mediated MPGN: facts and uncertainties. Kidney Int. 2020;98(5):1135-1148.
This content has been developed independently by Medthority who previously received educational funding in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
