ASN 2023: IgA nephropathy and other CMKDs
In this section
Emerging therapies for IgAN and PMN
The PROTECT trial pivotal findings
PROTECT is a phase 3, double-blind, active-controlled global clinical trial comparing the safety and efficacy of sparsentan, an orally active dual endothelin-1 angiotensin II receptor antagonist (DEARA), with irbesartan in people with IgA nephropathy (IgAN). Blocking both endothelin type A and angiotensin II type 1 receptors has been shown to have anti-inflammatory, antiproliferative and antifibrotic actions.
In this trial, Brad Rovin (The Ohio State University Wexner Medical Center, Columbus, USA) and colleagues randomly assigned 404 eligible participants to receive either sparsentan 400 mg (n=202) or irbesartan 300 mg (n=202) for 110 weeks.
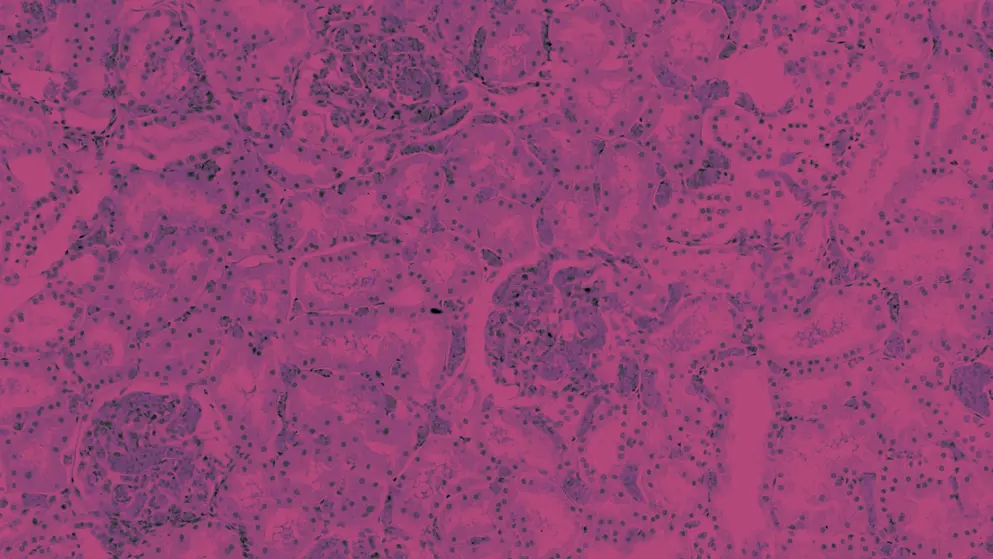
The primary efficacy endpoint was a change in urine protein-to-creatinine ratio (UPCR) from baseline to week 36. Secondary endpoints included estimated glomerular filtration rate (eGFR) slope and eGFR total slope taken at week 6 to 110, and day 1 to week 110, respectively; composite of kidney failure, defined as a 40% reduction in eGFR, end-stage kidney disease or all-cause mortality; and safety and tolerability. Baseline characteristics were comparable across groups and all participants had kidney biopsies that showed necropathy prior to the start of the study.
At the 36-week interim analysis, a significantly greater reduction in proteinuria was seen in the sparsentan group, compared with the irbesartan group (−49.8% vs −15.1%; P<0.001), amounting to a relative reduction of 41%. Sparsentan maintained a significant reduction in proteinuria throughout the course of the trial.
More participants on sparsentan achieved complete remission (urine protein excretion of <0.3 g/day) than those on irbesartan (31% vs 11%; relative risk, 2.5; 95% CI, 1.6–4.1).
While eGFR declined in both groups over the course of the trial, participants on sparsentan had better long-term kidney function preservation than irbesartan, with a mean change from baseline to week 110 of −5.8 for sparsentan and −9.5 for irbesartan. This meant that eGFR was 3.7 mL/min per 1.73 m2 higher with sparsentan than with irbesartan (95% CI, 1.5–6.0).
The progression to the composite endpoint occurred at a slower rate in the sparsentan group, compared with the irbesartan group. Treatment-emergent adverse events (TEAEs) and serious TEAEs were comparable between groups.
Overall, sparsentan met the primary endpoint and was well tolerated, with a safety profile comparable to that of irbesartan.
NeflgArd trial results
An oral, targeted-release (TR) capsule formulation of budesonide was designed specifically to treat patients with IgAN by inhibiting IgA production in Peyer’s patches. NeflgArd is a phase 3 clinical trial to determine the effects of TR budesonide 16 mg/day on eGFR change after 9 months of treatment and after 15 months of follow-up. The primary endpoint was the weighted average of eGFR over 2 years.
After 9 months, eGFR increased by 1.25% in those on TR budesonide but decreased by 8.2% in the placebo group. At 24 months, eGFR decreased by 11.0% in the TR budesonide group and by 21.5% in the placebo group.
Treatment with TR budesonide for 9 months resulted in approximately 50% less decline in kidney function, compared with placebo, after 2 years’ follow-up
Secondary endpoints demonstrated a 30% reduction in UPCR with TR budesonide use, compared with placebo, and this was sustained for 2 years. In addition, the time to the composite endpoint of a 30% reduction in eGFR or kidney failure was significantly delayed in the TR budesonide group, compared with the placebo group (HR, 0.45; 95% CI, 0.26–0.75; P=0.0014).
TR budesonide was well tolerated and had an expected safety profile for locally acting budesonide.
Richard Lafayette (Stanford University, California, USA) concluded that the findings from the NeflgArd trial suggest that TR budesonide treatment preserves kidney function and support its use as a disease-modifying therapy in people with IgAN.
Felzartamab in PMN: Final analysis of the M-PLACE trial
Felzartamab is an investigational, human IgG1 monoclonal anti-CD38 antibody that depletes plasmablasts and plasma cells. Targeting these cell types may reduce the level of phospholipase A2 receptor (PLA2R) autoantibodies and thereby prevent deposition of immune complexes in the basement membrane and epithelial podocytes, which in turn might prevent primary membranous nephropathy (PMN) progression.
Brad Rovin reported the results of M-PLACE, an open-label phase 1/2 trial assessing the safety, tolerability, pharmacokinetics and efficacy of felzartamab. Participants were recruited into one of two cohorts: those with newly diagnosed PMN or who had relapsed (cohort 1), and those who were refractory to prior immunosuppressive therapy (cohort 2). The primary endpoint was the incidence and severity of TEAEs.
TEAEs occurred in 87.1% of participants: 25.8% had any grade 3 or 4 TEAE; 16.1% had a serious TEAE; and 16.1% had a TEAE that led to treatment discontinuation. The most frequent TEAEs were infusion-related reactions. Hypogammaglobulinemia was also of interest as it occurred more frequently in cohort 1 than in cohort 2. Peripheral oedema was more prevalent in cohort 2.
After 1 week of treatment, the level of anti-PLA2R antibodies had decreased by 40% in 88% of participants. By the end of the trial, 65.4% of participants had reduced levels of anti-PLA2R, 30.8% had achieved immunologic complete response and 23.1% had achieved immunologic partial response. In addition, UPCR had decreased in most participants while serum albumin levels had increased; in 34%, these levels were within normal ranges. Treatment benefit waned in some participants in cohort 2, suggesting the need for a longer treatment duration.
Felzartamab had a favourable safety and efficacy profile, and further investigation is warranted for use as a therapeutic option for PMN
Targeted treatments for IgAN
Efficacy and safety of ravulizumab in IgAN
Primary analysis of a phase 2 randomised, double-blind, controlled trial to evaluate the efficacy, safety, pharmacokinetics and pharmacodynamics of ravulizumab, compared with placebo, in adults with IgAN garnered attention.
The primary endpoint was the percentage change in proteinuria from baseline to week 26, measured by urine protein (g/day) from the mean of two 24-hour collections, and a 24-hour UPCR.
Greater reductions in urine protein and UPCR were seen in participants treated with ravulizumab, compared with those who received placebo:
- 24-hr urine protein (g/day) treatment effect of −8% (90% CI, −45.5 to −9.7; P=0.0059)
- 24-hr UPCR (g/g) treatment effect of −1% (90% CI, −47.5 to −14.7; P=0.0012)
Secondary endpoints were spot UPCR, which showed a rapid and clinically meaningful reduction in proteinuria at 26 weeks, and eGFR, which was stable with ravulizumab, compared with placebo.
There were no apparent adverse events of special interest (meningococcal infections) or death that occurred, nor were there any discontinuations due to adverse events or ravulizumab treatment.
Sibeprenlimab in patients with IgAN: A phase 2 trial
A phase 2 double-blind, placebo-controlled study was performed to determine the efficacy and safety of sibeprenlimab, a humanised IgG2 monoclonal antibody known to bind and block APRIL. Participants with IgAN and a high risk of progression despite standard-of-care treatment were included in the trial.
Treatment with sibeprenlimab for 12 months led to a significant reduction in proteinuria as shown by a change in the log-transformed 24-hour UPCR from baseline to month 12 (P=0.0002), with geometric mean ratio reduction of 47.2%, 58.8% and 62.0% for sibeprenlimab 2, 4 and 8 mg/kg, respectively, and 20% for placebo groups.
In addition, stabilisation of eGFR decline, robust suppression of Gd-IgA1 and IgA, and reduction of serum APRIL were seen with sibeprenlimab. IgG and IgM levels were also reduced by 35% and 75%, respectively.
Sibeprenlimab demonstrated an acceptable safety profile, with the incidence of TEAEs similar between groups and with no increased risk of infection or infestations.
A phase 3 investigation (VISIONARY) is currently underway to further investigate the efficacy and safety of sibeprenlimab in a larger IgAN population.
IMAGINATION: A global phase 3 trial of RO7434656 in IgAN
IMAGINATION is a phase 3 double-blind, placebo-controlled trial evaluating the efficacy, safety, and pharmacokinetics of RO74346456, a ligand-conjugated antisense oligonucleotide, in biopsy-confirmed primary IgAN. RO74346456 binds to and destroys complement factor B mRNA, preventing the production of factor B protein, a key protease necessary for the activation and amplification of the alternative complement pathway.
Participants will be randomised 1:1 to either RO74346456 or placebo administered as a subcutaneous injection every 4 weeks for 105 weeks.
The primary endpoint is the change in proteinuria from baseline as measured by geometric mean change of UPCR at week 37 from a 24-hour collection. Secondary endpoints include the total eGFR slope at week 105, change in symptoms and health-related quality of life at week 105, time to first composite kidney failure endpoint, change in fatigue at week 105, plasma concentrations of RO74346456, and incidence and severity of TEAEs.
Preliminary findings from SPARTAN
SPARTAN is a phase 2, open-label, single-arm trial investigating the safety, efficacy, and mechanism of action of the DEARA sparsentan as a first-line therapy in people newly diagnosed with IgAN. Sparsentan was granted accelerated approval in the USA for the treatment of people with IgAN at risk of disease progression, based on improvements in proteinuria demonstrated in the ongoing phase 3 PROTECT trial.
Preliminary results demonstrated rapid and sustained reductions in proteinuria with a ~60% reduction from baseline after 4 weeks of sparsentan treatment. Both eGFR rates and blood pressure remained stable over 36 weeks. Mean body weight showed minor fluctuations while mean total body water showed modest reductions from baseline.
Sparsentan was generally well tolerated, with three SAEs occurring – none of which were related to treatment.

